Georgia’s 2023 Health Budget
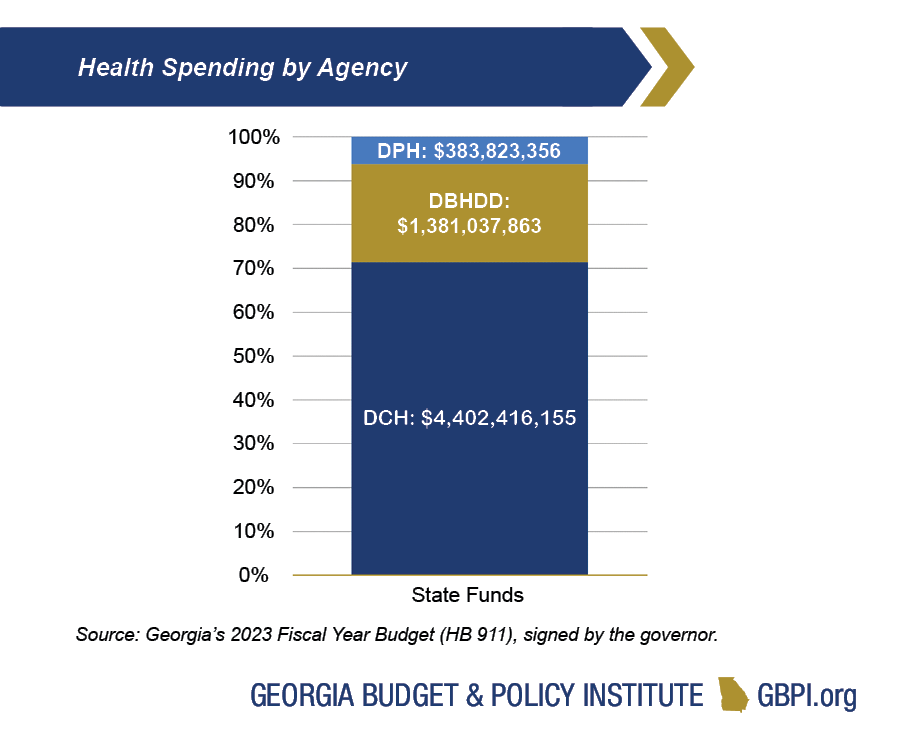
The Departments of Behavioral Health and Developmental Disabilities, Community Health and Public Health are the three primary agencies focused on the state’s health care and public health systems. Georgia plans to provide $6.2 billion in total state funds for these three agencies in the 2023 budget year, or about 20 percent of overall state spending. General Fund appropriations account for $5.5 billion, or about 89 percent, of the total state funds for these three agencies; other sources, like tobacco settlement funds, account for the remaining $708 million of state health spending. General Fund dollars for these three agencies increased by $559 million from 2022 to 2023.
A resilient Georgia must have the capacity to recover and adjust amid fresh challenges and ever-shifting conditions. The COVID-19 pandemic has shown us that a flexible, well-resourced and integrated public health infrastructure and health care system is a key building block for a more resilient Georgia. Unfortunately, Georgia’s health system performance consistently ranks near the bottom, and Georgia was ranked 47th in how our health systems responded to the pandemic—based on measures like hospital and intensive care unit capacity, vaccination rates, and COVID-19 death rates. Increasing our investment in our state health agencies can prepare us for the next health emergency.
The Department of Community Health (DCH) accounts for $4.4 billion, or 71 percent, of total state health spending. It operates Georgia’s Medicaid and PeachCare programs, conducts some planning and regulatory functions and administers the State Health Benefit Plan that provides health care to teachers and state employees.
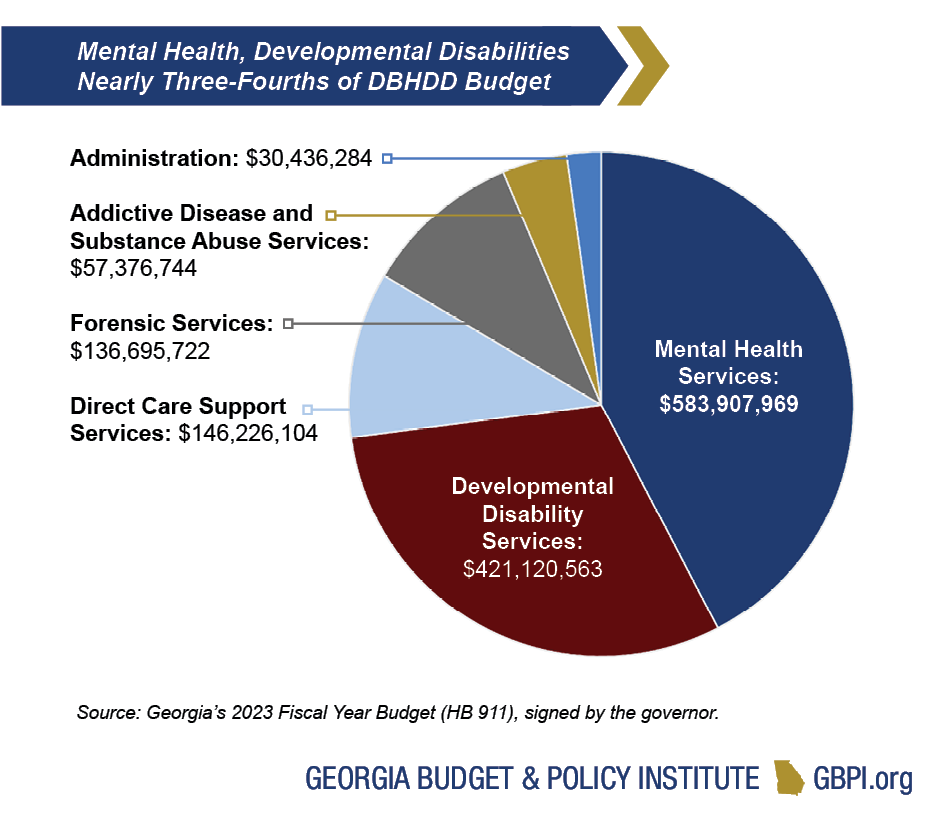
The Department of Behavioral Health and Developmental Disabilities (DBHDD) accounts for $1.4 billion, or 22 percent, of total state spending on health. This includes some services funded through federal Medicaid dollars, but largely relies on state funds to provide services for uninsured and underinsured Georgians living with behavioral health conditions and/or developmental disabilities.
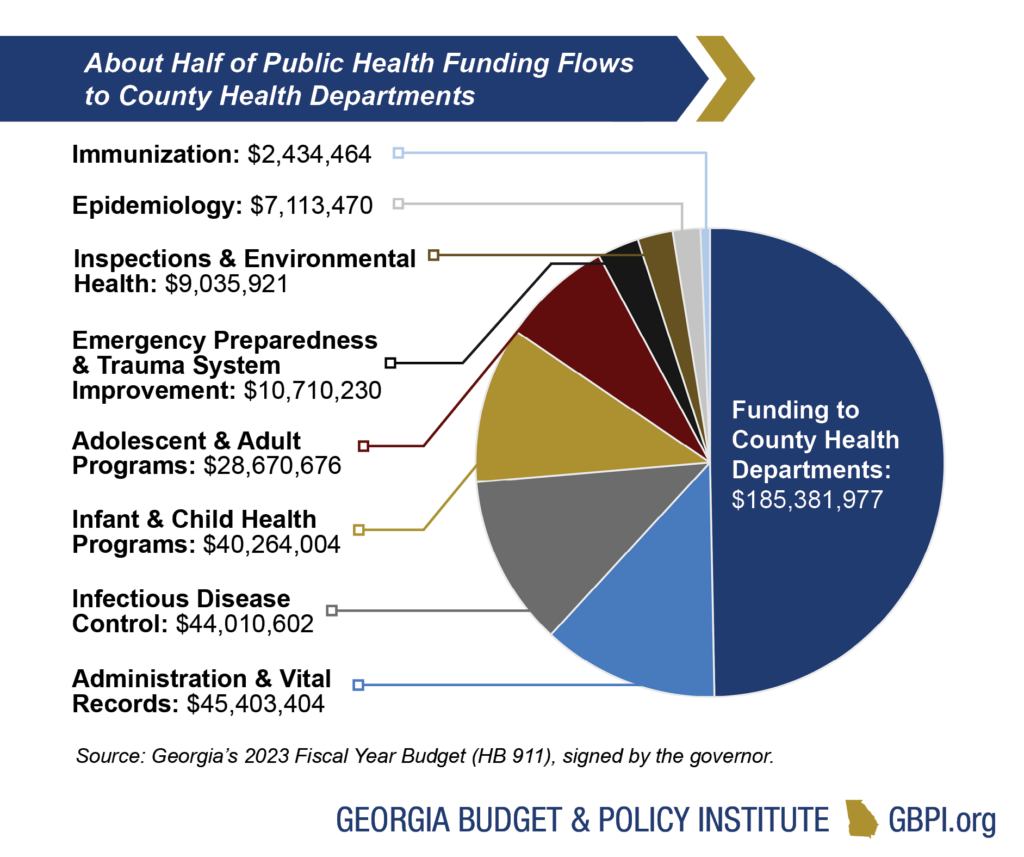
The Department of Public Health (DPH) accounts for $384 million, or about 6 percent, of total state spending on health. It operates a variety of population-based programs, such as immunizations, infectious disease control and health promotion.
Unequal Access to Health Care
Georgia continues to be impacted by unequal access to affordable, high-quality health care. Historically, Georgia has ranked near the bottom in terms of Medicaid spending per enrollee. Georgia spent about $5,037 per full benefit enrollee compared to the United States average of $7,106 in 2019 (the most recent data available). Georgia expects to spend $4.1 billion in state funds in 2023 to serve Georgians covered by Medicaid. The 2023 budget reflects some modest increases in Medicaid reimbursement—for example, $10.7 million for reimbursement of therapeutic services.
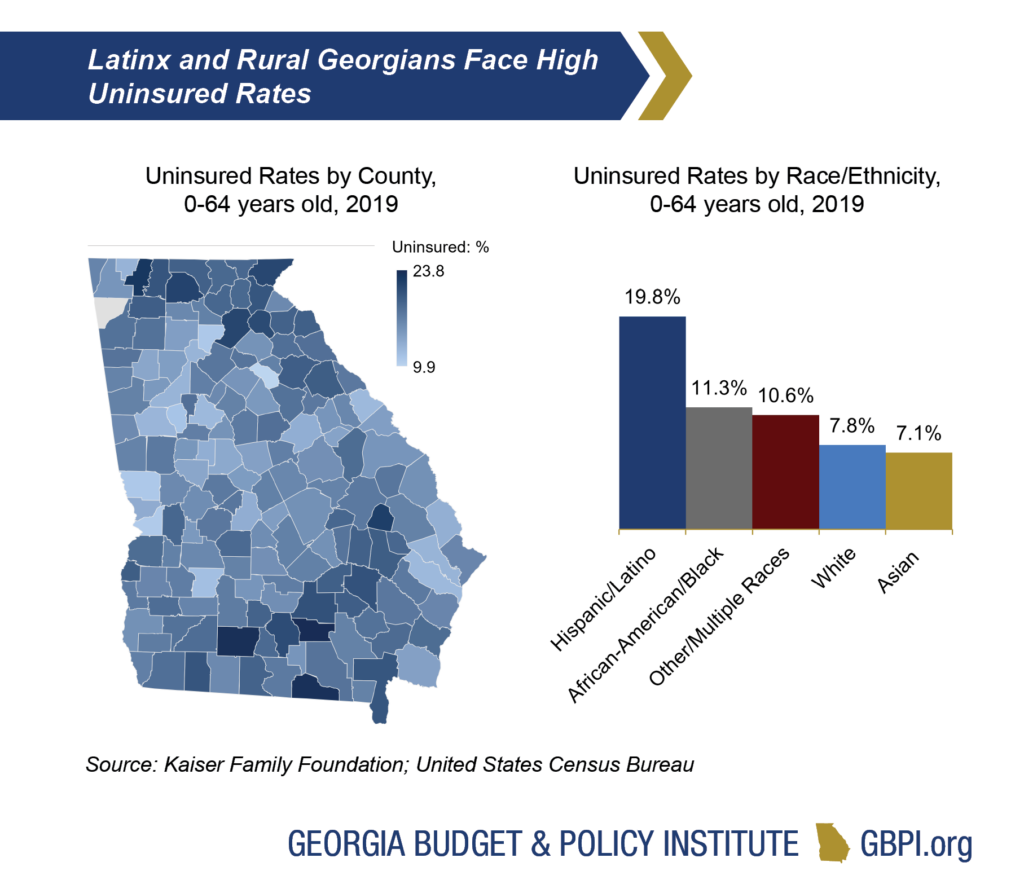
Ranking third nationally in the number of uninsured people, Georgia continues to struggle with the impact of not expanding Medicaid—a decision that reflects an inequitable distribution of power and history of oppression. While more than 1 in 10 Georgians do not have health care coverage, the burden is heaviest on Georgians living in rural communities and Georgians of color—particularly Latinx Georgians.
Medicaid and PeachCare Enrollment Spending
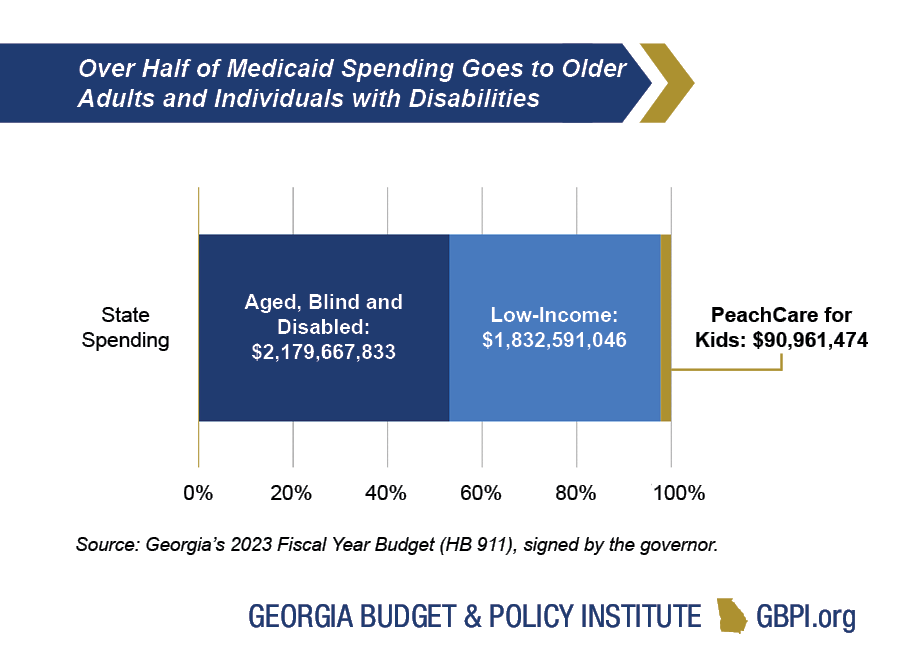
Medicaid and PeachCare serve about 2.3 million Georgians, or about 1 in 5 residents. Low-income Medicaid serves children, pregnant women and some parents with very low incomes. The Aged, Blind and Disabled portion of the program serves older adults with low incomes and people with physical and developmental disabilities.
Medicaid is the main source of health coverage for Georgians with long-term health care needs, both in nursing homes and in community-based settings. Medicaid also helps pay Medicare premiums for more than 258,000 Georgians aged 65 and older and younger adults with long-term disabilities.
Medicaid and PeachCare cover about 1.6 million children—representing almost 70% of Medicaid beneficiaries in the state. Medicaid also pays for more than half of Georgia births. PeachCare is a separate program serving children from families with incomes above the Medicaid threshold, but who often lack access to other forms of coverage.
Medicaid Provides Flexibility to Meet Critical Health Needs
Medicaid is a partnership between the state and federal government, with the federal government paying about 66 percent of the state’s total Medicaid costs. This federal support is beneficial for the states when facing emergencies or economic downturns, and the federal government can provide relief by paying more or giving states the opportunity to test
new approaches.
Since the beginning of the COVID-19 pandemic in March 2020, Georgia has received more federal money for Medicaid (a higher matching rate of 72 percent) and has not been allowed to disenroll anyone. That means that millions of Georgians have had uninterrupted access to affordable health care coverage during a time of widespread health and economic instability. Georgia also saw about $544 million in savings in last year’s budget thanks to the enhanced federal match and will continue to produce savings in the 2023 budget year.
Georgia is taking advantage of the flexibility provided by the federal Medicaid program to better serve Georgia’s pregnant women and children. The 2023 budget includes about $28 million to extend Medicaid coverage to birthing parents for up to one year after the end of pregnancy. The 2023 budget also includes $39 million in state funds for the implementation of express lane enrollment, which can help uninsured children get streamlined access to Medicaid and PeachCare by using eligibility findings from other programs, like Supplemental Nutrition Assistance Program (SNAP), to do automatic enrollments and renewals.
Access to affordable health care—including behavioral health care—is a critical component of one’s overall resilience. Unfortunately, thousands of Georgians fall into the coverage gap with incomes too high for Georgia’s Medicaid eligibility but too low to qualify for marketplace subsidies. Overdose and suicide are the 1st and 5th leading Georgia causes of early death, and more than 1 in 4 Georgians in the coverage gap are believed to have a behavioral health condition.
States that expanded Medicaid have improved access to behavioral health care; lowered rates of suicide; and reduced stress among people with low incomes. Expanding Medicaid can also boost the behavioral health workforce.
Through the Mental Health Parity Act, Georgia made a historic step forward to improving the lives of Georgians living with behavioral health conditions. Fully expanding Medicaid could build upon that momentum by closing the coverage gap and delivering behavioral healthcare to more Georgians.
The Year of Mental Health
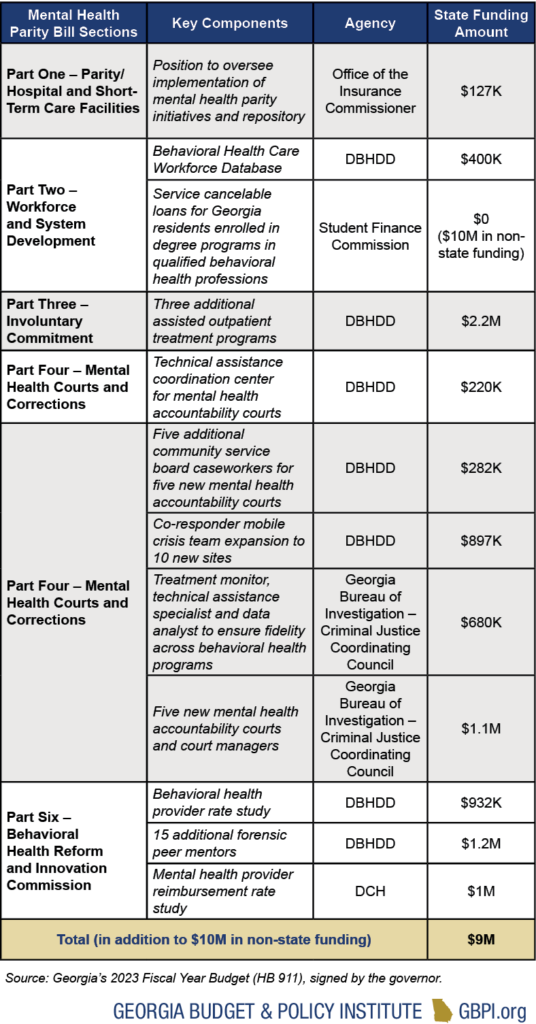
In 2019, state legislators convened the Behavioral Health Reform and Innovation Commission, and, in 2022, House Speaker David Ralston introduced legislation that built upon the findings of that commission and declared that “no issue is more important to me this session than mental health.” That legislation, known as the Mental Health Parity Act, passed with unanimous bipartisan support.
The bill itself is expansive with provisions that touch on everything from police-mental health co-response teams to workforce development to assisted outpatient treatment. One of the centerpieces is the first section of the bill on mental health parity, which requires insurers to treat mental health as they do physical health.
The 2023 budget includes funding that corresponds to key components of that bill, and the table below highlights some of that funding.
Behavioral Health and Developmental Disabilities
The Department of Behavioral Health and Developmental Disabilities (DBHDD) operates state hospitals and provides community-based services through contracted providers to Georgians living with mental health conditions, substance use disorders and/or developmental disabilities. The department also operates programs for forensic evaluation and treatment under the court system’s jurisdiction.
Georgia plans to dedicate almost $1.4 billion in General Funds along with $10 million in Tobacco Settlement Funds to DBHDD, a $122 million increase in state funding compared to 2022.
Public Health
The Department of Public Health (DPH) operates programs focused on disease and injury prevention, health promotion, and health-related disaster response and preparedness. The department receives almost $357 million from the General Fund and $14 million in Tobacco Settlement funds. The largest state-funded programs provide funding to 159 county health departments, help prevent the spread of infectious disease and provide services for children. The department’s 2023 budget increased by $48 million compared to 2022.
Georgia’s public health programs also receive federal support. Federal money comprises 50 percent of the department’s $792 million budget, while state and other funds comprise the rest. Of those federal funds, more the half is accounted for by the program known as WIC, which provides supplemental food, breastfeeding support, information on healthy eating, and referrals to health care for pregnant and postpartum women and children up to age five.
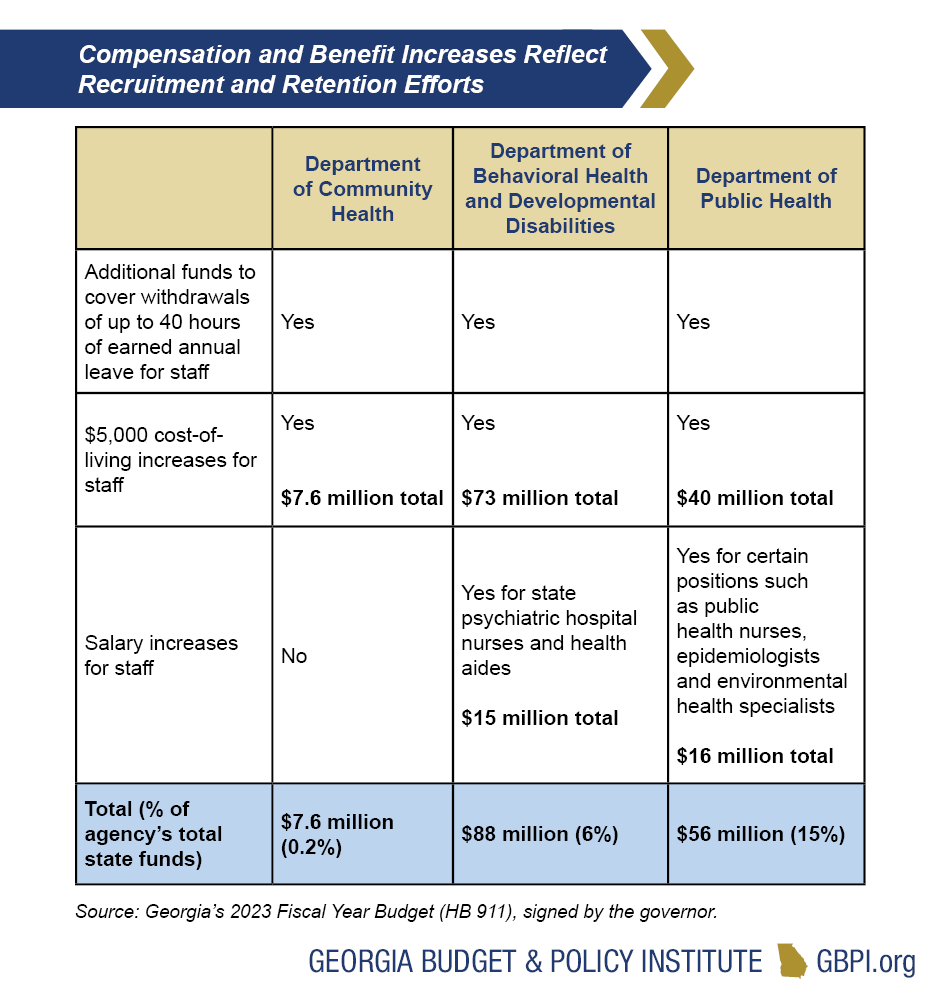
Budget Reflects Health Agencies’ Recruitment and Retention Needs
Like other states, Georgia’s health agencies have experienced significant staffing shortages over the past two years, and the 2023 budget reflects efforts to address recruitment and retention. While the increases are encouraging, additional investments are needed to ensure that compensation is competitive and that the state’s health agencies can fully staff critical positions. For example, environmental health specialists, who perform a diverse array of vital functions from food safety inspections to home-based lead investigations, will receive a much-needed salary increase that is still just 85% of the market average.