Georgia’s 2024 Health Budget
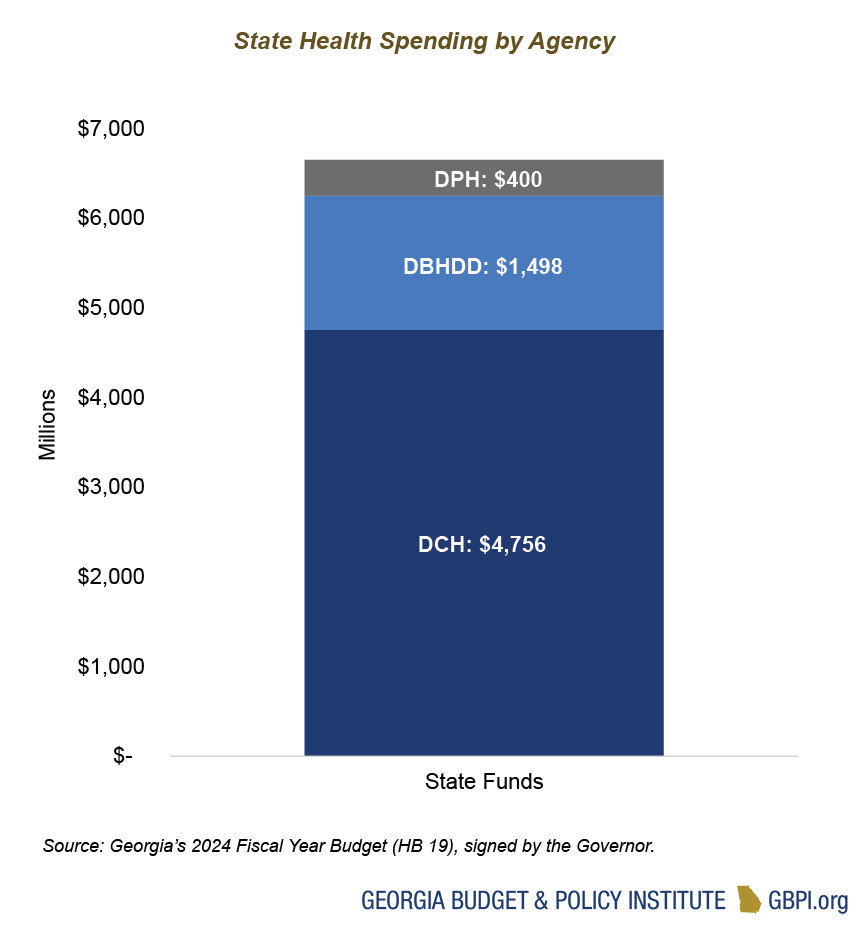
The Departments of Behavioral Health and Developmental Disabilities, Community Health and Public Health are the primary agencies focused on the state’s health care and public health systems. Georgia plans to provide $6.7 billion in state funds for these three agencies in the fiscal year (FY) 2024 budget year, or about 21 percent of overall state spending. General Fund appropriations account for $5.9 billion, or about 89 percent, of the total state funds for these three agencies. Other sources, like Tobacco Settlement Funds, account for the remaining $712 million of state health spending. General Fund dollars for these three agencies increased by $638 million, or about 11 percent, from the AFY 2023 budget.
The Department of Community Health (DCH) accounts for about $4.8 billion, or 71 percent, of state health spending. The Department of Behavioral Health and Developmental Disabilities (DBHDD) accounts for about $1.5 billion, or 23 percent, of state spending on health. The Department of Public Health (DPH) accounts for $400 million, or about 6 percent, of state spending on health.
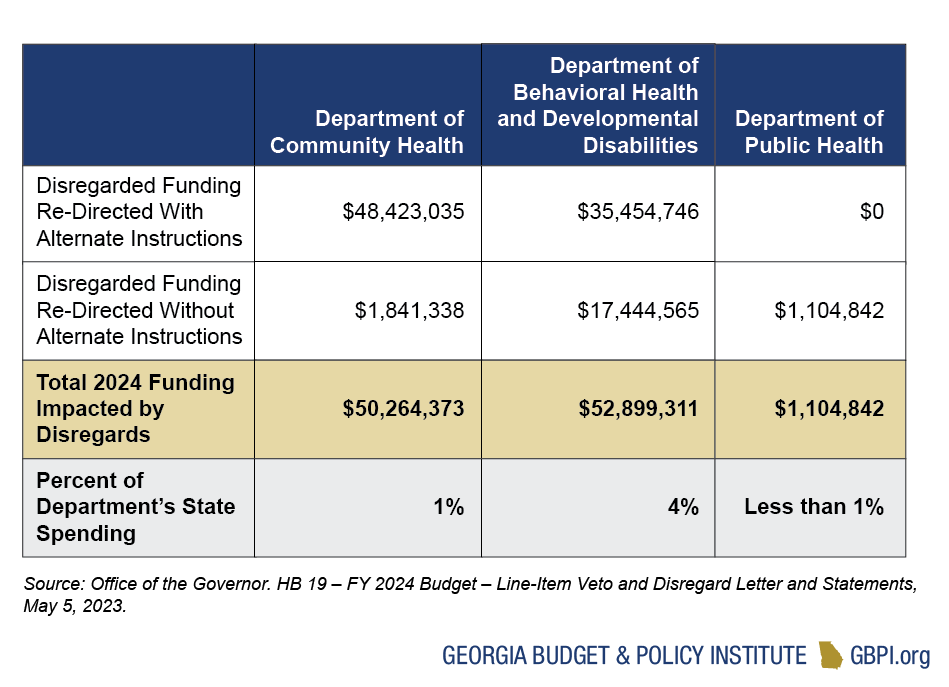
Health Priorities Impacted by Governor’s Directive to Disregard Budget Language
In May 2023, in his review and approval of the FY 2024 budget, the Governor issued guidance directing state agencies to disregard some budget language and to consider that language non-binding. In total, the Governor is directing state health agencies to disregard about $104 million in funding along with seven additional budget actions with no associated FY 2024 funding (also known as ‘Yes’ line items). These disregards are a small proportion of each Department’s budget but represent significant changes to address pressing needs like workforce gaps. For DCH, most of the disregards impact Medicaid provider reimbursement rate increases—from home and community-based services to obstetrics and gynecology rate increases. Due to concerns about a Medicaid base funding deficit, the Governor has redirected that funding to be used instead for Medicaid spending and growth.
For DBHDD, much of the disregarded funding for annualizing NOW/COMP waiver slots (to expand home- and community-based services and supports for individuals with disabilities) and for behavioral health crisis centers is still available for agency use with slightly modified language. However, about $17 million in funding for various purposes—from increasing salaries for state psychiatric hospital nurses and health aides to supporting the 988 suicide and crisis lifeline—has been entirely disregarded.
Georgians Face Inequitable Access to Care
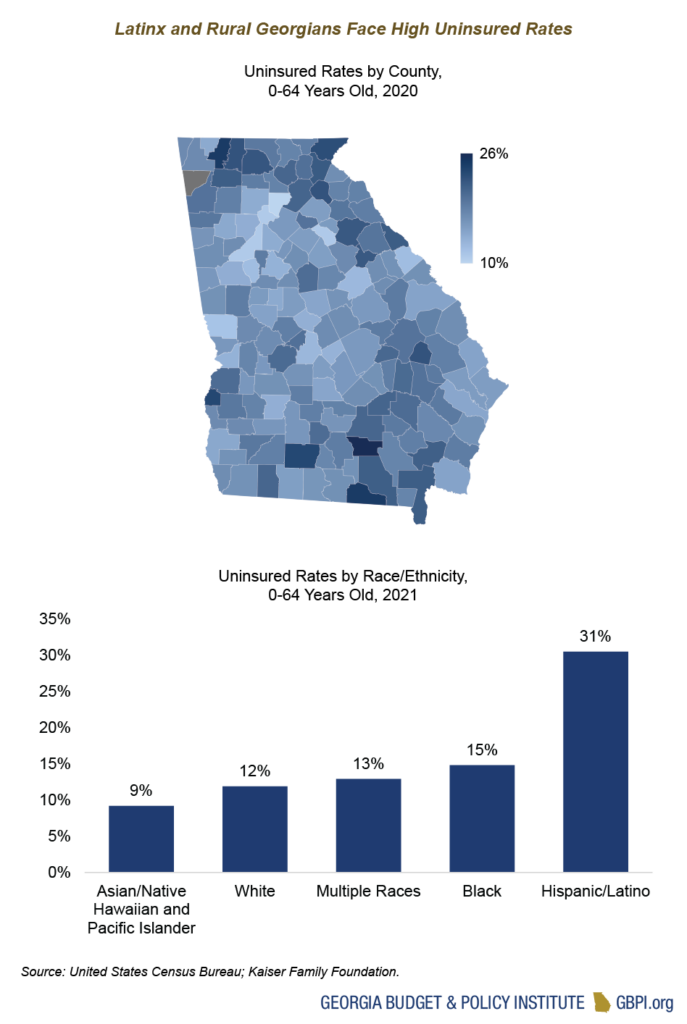
Unequal access to affordable, high-quality health care continues to impact Georgians. Ranking third nationally in the number of uninsured people, the state’s decision not to fully expand Medicaid reflects its history of oppression and an imbalanced power structure. While more than 1 in 8 Georgians does not have health care coverage, the burden is heaviest on Georgians living in rural communities and Georgians of color—particularly Latinx Georgians.
Georgia also ranks near the bottom for Medicaid spending per enrollee. On average, Georgia spent about $5,953 per full benefit enrollee compared to the United States average of $9,303 in 2020 (the most recent data available). Children make up a majority of Georgia’s Medicaid and PeachCare population, and the state spends about $2,426 per child enrollee—the second lowest in the nation. Georgia expects to spend $4.4 billion in state funds in FY 2024 to serve Georgians who are covered by Medicaid or PeachCare. Of note, the FY 2024 budget includes about $584,000 to allow pregnant women and children who are lawful permanent residents to enroll in Medicaid/PeachCare without waiting five years. This small investment unlocks access to health care for new Georgians during the pivotal pregnancy, postpartum and childhood years.
Medicaid and PeachCare Enrollment and Spending
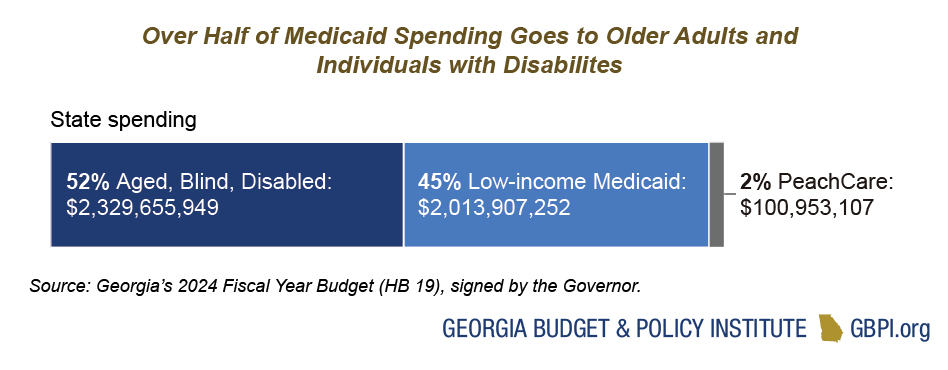
Medicaid and PeachCare serve about 3 million Georgians, or about 1 in 4 residents. Low-income Medicaid serves children, pregnant and postpartum people, and some parents with very low incomes. The Aged, Blind and Disabled portion of the program serves older adults with low incomes and people with physical and developmental disabilities. PeachCare is a separate program serving children from families with incomes above the Medicaid threshold, but who often lack access to other forms of coverage.
About 46 percent of Georgia births are financed by Medicaid, and almost 70 percent of Medicaid and PeachCare beneficiaries in the state are children. Medicaid is also the main source of health coverage for Georgians with long-term health care needs, both in nursing homes and in community-based settings. Medicaid helps pay Medicare premiums for more than 268,000 Georgians aged 65 and older and younger adults with long-term disabilities.
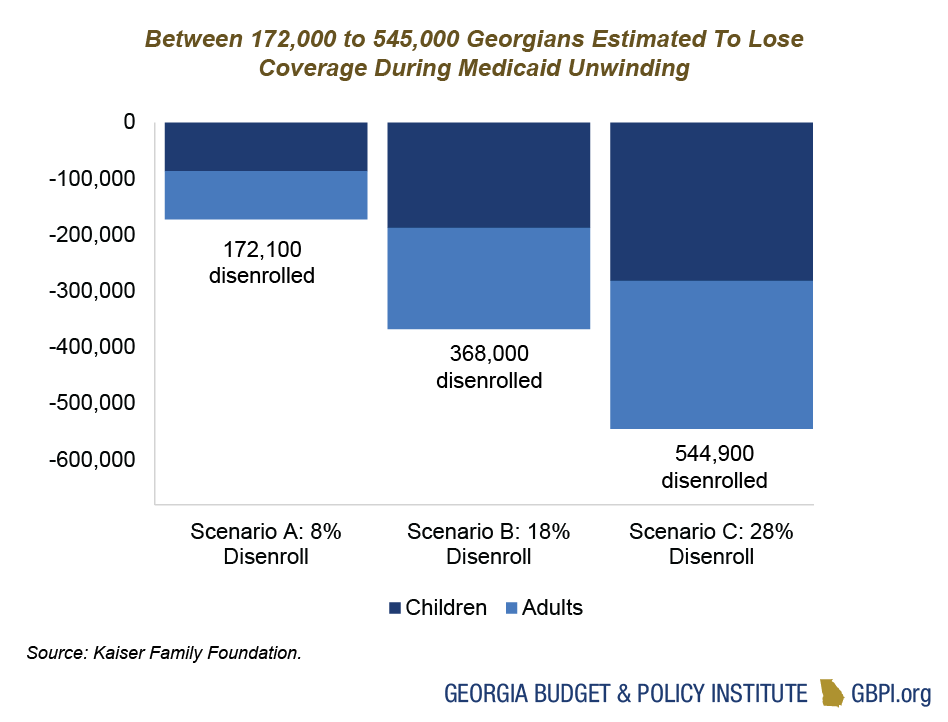
Georgians—Particularly Children and Families of Color—At Risk of Losing Coverage During Medicaid Unwinding
Thanks to a pandemic-era policy, millions of Georgians have had uninterrupted access to affordable health care over the past three years—allowing them to see a doctor, refill prescriptions and get vaccines during a time of health and economic uncertainty. Starting in April 2023, that continuous Medicaid and PeachCare coverage began to unwind, and every child and adult enrolled in Georgia’s health care safety net will have their eligibility re-determined prior to the end of May 2024. This unprecedented health care event will put pressure on state agencies and jeopardize the health and financial security of Georgians with lower incomes. Hundreds of thousands of Georgians will lose coverage. An estimated 45 percent of those losing coverage will be impacted by procedural denials, which means they are still eligible but are denied coverage due to a human or technological error in the process—like the form being sent to the wrong address. The burden of this health care coverage loss will likely fall heaviest on children, young adults and postpartum people from communities of color.
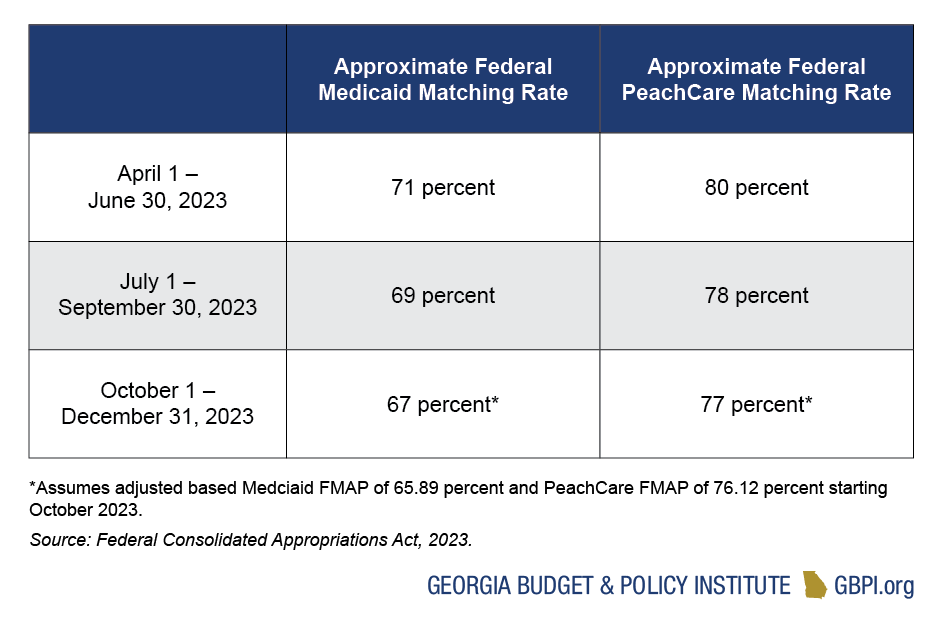
Georgia will Continue to Receive Additional Federal Funding to Cover Medicaid Enrollees Through End of 2023
In exchange for keeping Georgians continuously enrolled in Medicaid since the pandemic started, Georgia has received an enhanced Federal Medical Assistance Percentage (FMAP). Medicaid is a partnership between the state and federal government, and the FMAP determines the amount the federal government pays to the state for providing Medicaid services. The federal government gradually began decreasing the pandemic-related enhanced FMAP in April. Although the Medicaid unwinding period extends through May 2024, Georgia will go back to its standard FMAP of about 66% in January 2024. Medicaid unwinding is likely to result in significant declines in enrollment and, in turn, decreased total Medicaid spending. As the process unfolds, further adjustments to the budget will likely be needed to balance enrollment reductions and FMAP cuts.
Investments in the Governor’s Health Care Expansion Plan for Low-Income Georgians
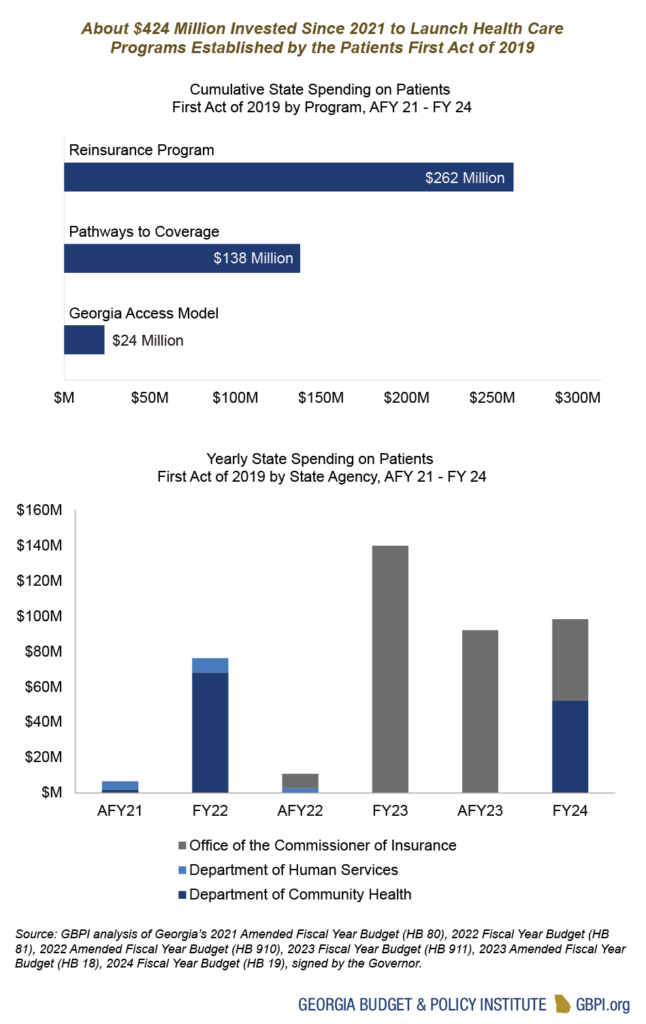
In 2019, the passage of the Governor’s signature health care legislation, the Patients First Act or SB 106, paved the way for Georgia to seek federal approval for three new programs:
- The Georgia Pathways to Coverage program, which proposes to partially expand Medicaid eligibility to low-income adults who meet work or other monthly reporting requirements;
- The Georgia Reinsurance Program, which establishes a claims-based reinsurance program to help offset costs of enrollees in the individual health insurance market who have large medical claims; and
- The Georgia Access Model, which would remove the state from the federal marketplace (often referred to as HealthCare.gov) without a state-based alternative. With the passage of SB 65 during the 2023 Legislative Session, the state has pivoted away from the original Georgia Access Model plan and moved toward a state-based health insurance exchange. Going forward, the program will be funded by user fees rather than state General Funds.
Overall, the state has made a significant investment in all three programs. The Pathways to Coverage Program and Georgia Access Model’s state-based exchange are set to launch in 2023, and the Reinsurance Program launched in 2022. It will be important to track the impact of these investments on increasing access to affordable, high-quality health care.
FY 2024 Budget for Pathways to Coverage Program Falls Short
This budget year, the state is set to launch the Pathways to Coverage program. This program expands health care coverage for low-income adults who are currently in the coverage gap, meaning that they earn too much to qualify for traditional Medicaid coverage but not enough to qualify for subsidized coverage in the health insurance marketplace (or HealthCare.gov). This program does not impose new requirements on Georgians already covered under traditional Medicaid eligibility, such as older adults over 65 years old or pregnant and postpartum people. Instead, this program expands coverage to Georgians ages 19 – 64 years old who have a household income of up to 100 percent of the federal poverty level. To be eligible, enrollees must complete and report a minimum of 80 hours per month of qualifying activities like employment, community service or higher education.
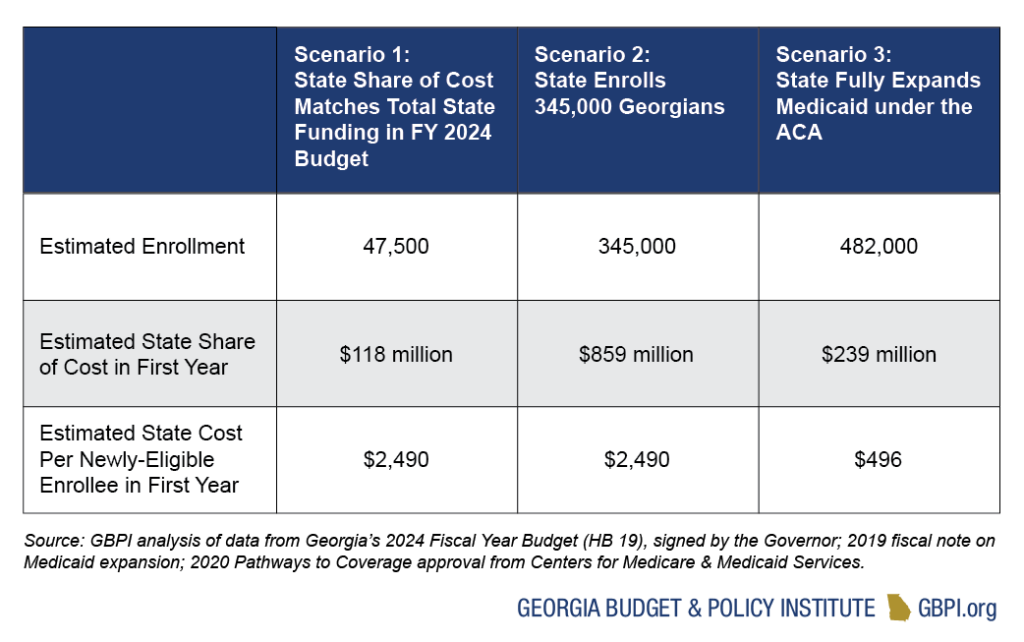
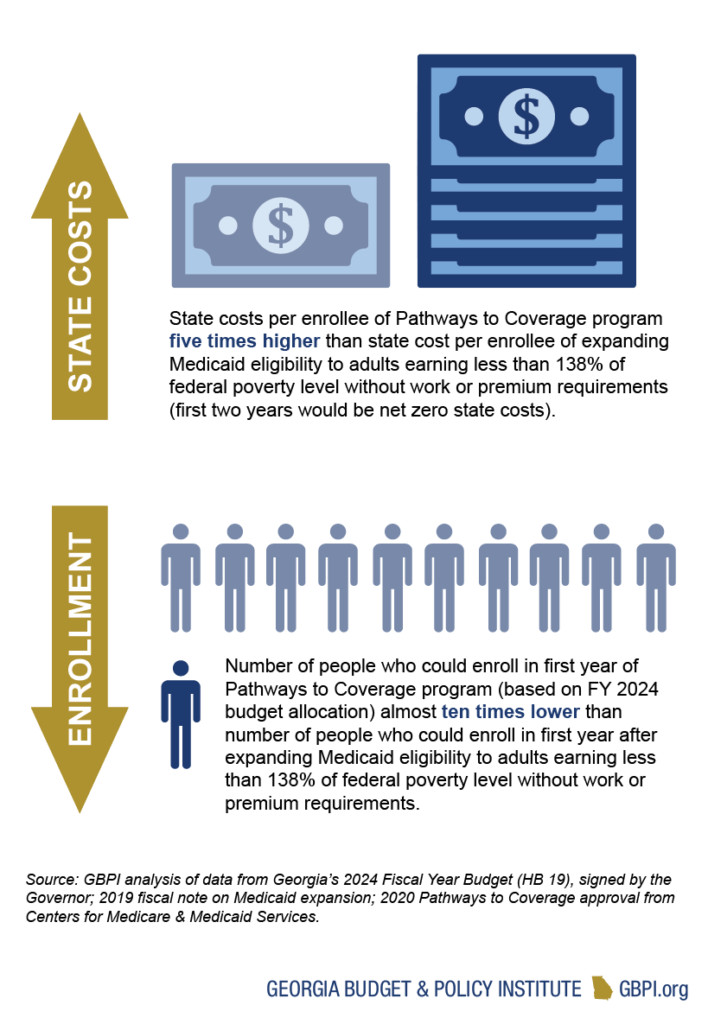
The FY 2024 budget includes $52 million in 2024 state funds and recognizes $65.5 million in unused 2022 state funds (about $118 million in total state funds). Based on GBPI analysis, the total state funds allotted for the Pathways to Coverage program in the FY 2024 budget will allow the state to enroll about 47,500 Georgians—far fewer than the 345,000 Georgians that the Governor said are qualified for the program in his 2023 State of the State address. By contrast, if the state expands Medicaid eligibility to low-income adults without arbitrary restrictions or burdensome reporting requirements, the state could cover almost 500,000 Georgians at a much lower cost. In fact, the temporary financial incentives offered under the American Rescue Plan would make the state cost of full expansion net zero for the first 2 years.
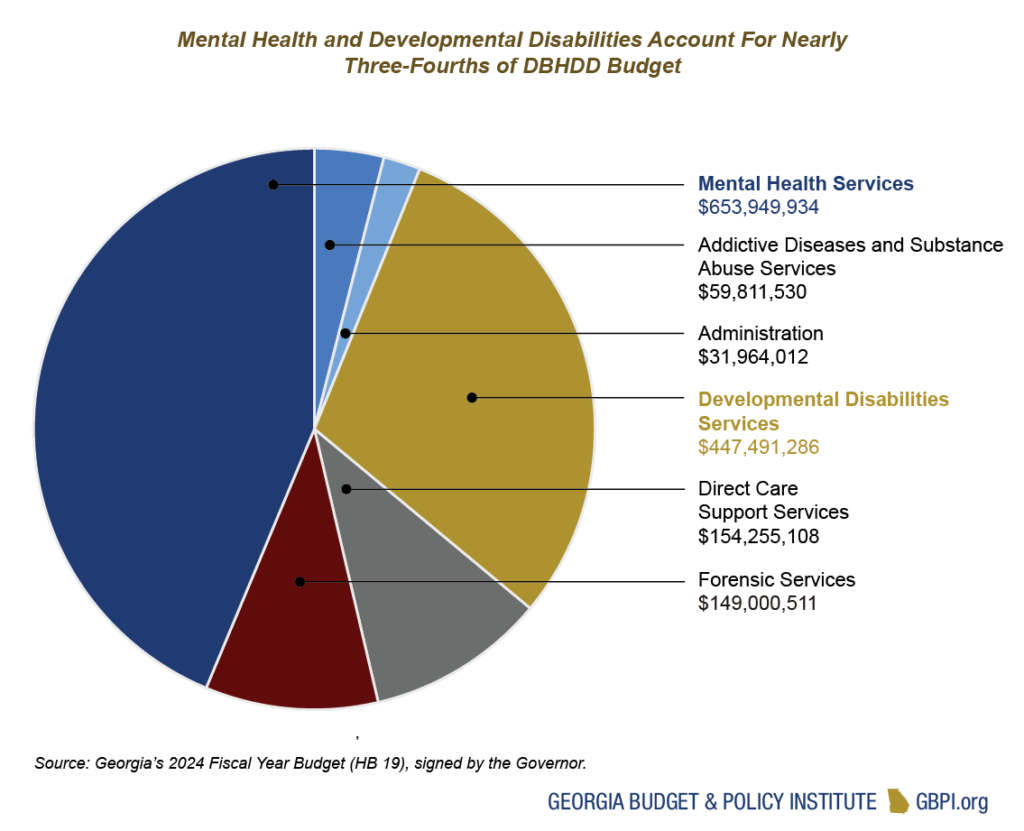
Behavioral Health and Developmental Disabilities
The Department of Behavioral Health and Developmental Disabilities (DBHDD) provides services primarily for uninsured and underinsured Georgians living with mental health conditions, substance use disorders and/or developmental disabilities. It operates state hospitals and provides community-based services through contracted providers. The department also operates programs for forensic evaluation and treatment under the court system’s jurisdiction. Georgia plans to dedicate almost $1.5 billion in General Funds along with $10 million in Tobacco Settlement Funds to DBHDD. Total state spending for DBHDD in FY 2024 represents an increase of almost 8 percent over the AFY 2023 budget.
Public Health
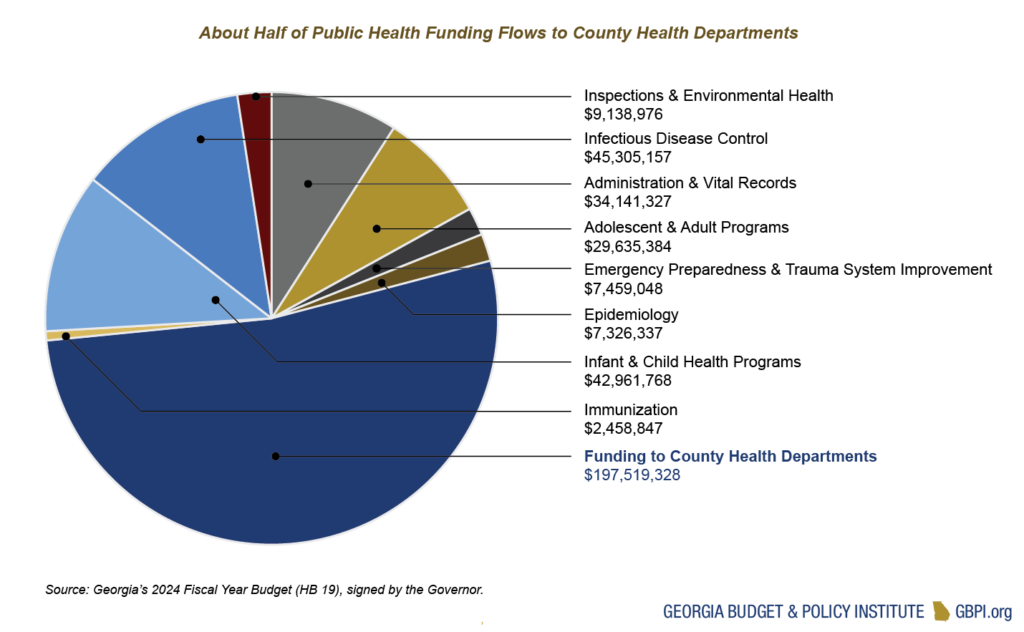
The Department of Public Health (DPH) operates programs focused on disease and injury prevention, health promotion and health-related disaster response and preparedness. The department receives about $369 million in General Funds and almost $14 million in Tobacco Settlement funds. The largest state-funded programs provide funding to 159 county health departments, help prevent the spread of infectious diseases and provide services for children. Total state spending for DPH in FY 2024 represents an increase of 5 percent over the AFY 2023 budget.
Georgia’s public health programs also receive substantial federal support. Federal money comprises almost half of the department’s $806 million budget, while state and other funds comprise the rest. Of those federal funds, more the half is accounted for by the Special Supplemental Nutrition Program for Women, Infants, and Children (or WIC), which provides low-income pregnant and postpartum people and children up to age five with healthy food, nutrition information, breastfeeding support and other services.
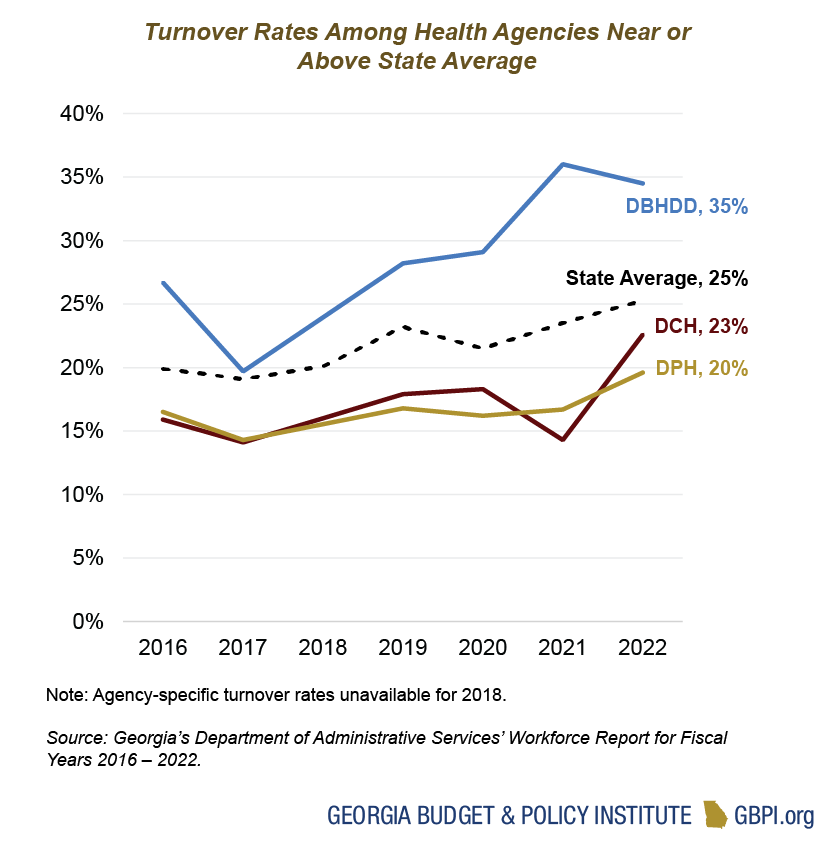
Workforce Recruitment and Retention Remain an Issue for State Health Agencies
Turnover rates for the state’s health agencies have increased since 2016, ranging from about 20 percent for DPH to about 35 percent for DBHDD. DBHDD has seen a 28 percent decrease in staff from 2016 to 2022—from a high of about 4,128 full-time staff to a low of 2,982. Similarly, DCH has seen a 32 percent decrease in staff from 2016 to 2022—from a high of about 943 full-time staff to a low of 641. The AFY 2023 budget included $5,000 cost-of-living increases, as well as salary increases for select job categories at both DBHDD and DPH. The impact of those increases is not reflected in the most recent workforce data. Full-time staff at all three agencies will receive an additional $2,000 cost-of-living increase as part of the FY 2024 budget. Even after these adjustments take effect, continued efforts will likely be needed to ensure that our state’s agencies are fully staffed with a trained, diverse, stable workforce that is ready to meet Georgia’s ever-shifting health needs.