Georgia’s 2022 Health Care Budget
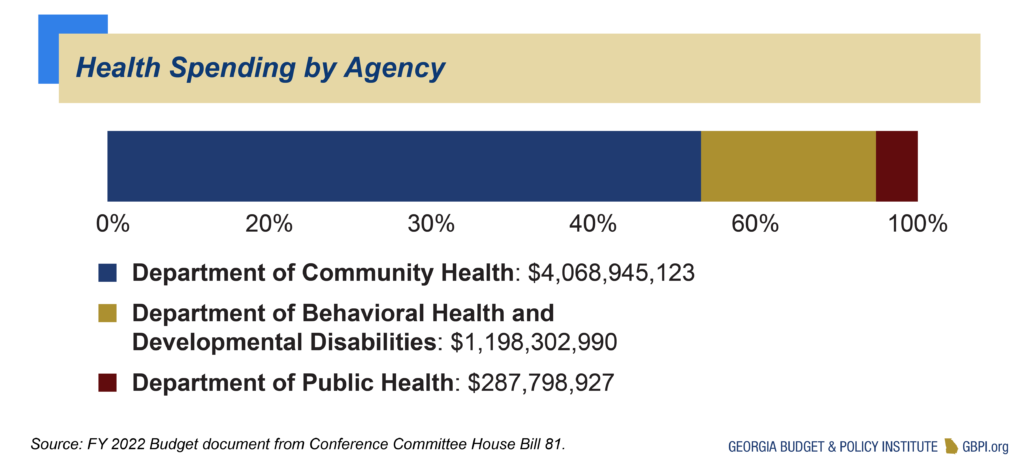
The Departments of Community Health, Behavioral Health and Developmental Disabilities and Public Health are the three primary agencies focused on the state’s health care and public health systems. Georgia plans to provide $5.6 billion in total state funds for these three agencies in the 2022 budget year, or about 20 percent of overall state spending. General Fund appropriations for these agencies account for $4.9 billion, or 87 percent of total state funds, while other sources account for about $696 million. General Fund dollars for these three agencies increased by $409 million from 2021 to 2022.
The Department of Community Health (DCH) accounts for $4.1 billion, or 73 percent, of total state spending on health care. It operates Georgia’s Medicaid and PeachCare programs, conducts some planning and regulatory functions and administers the State Health Benefit Plan that provides health care to state employees and teachers. Funding for the state health plan comes from school districts, state agencies and their employees and retirees.
Georgia plans to spend about $1.2 billion, or 22 percent of Georgia’s 2022 health care expenses, on behavioral health and services for people with developmental disabilities. This includes some services funded through Medicaid, but largely relies on general funds to provide services for uninsured and underinsured Georgians.
The Department of Public Health (DPH) operates a variety of population-based programs such as immunizations, health screenings and infectious disease control. It receives $288 million, or about 5 percent of Georgia’s 2022 health spending.
Medicaid and PeachCare Enrollment and Spending
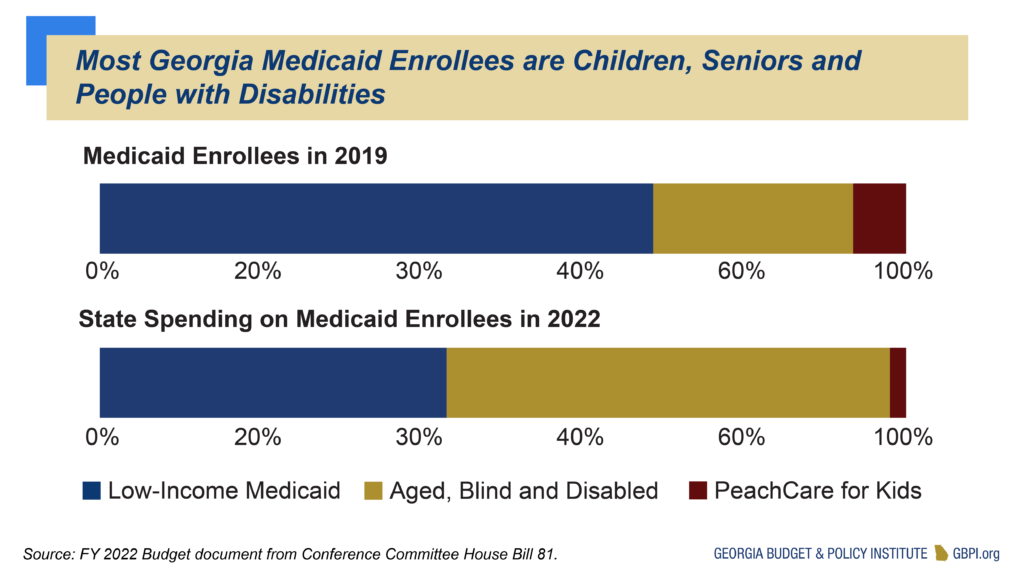
Medicaid and PeachCare serve about 2 million Georgians, or 1 in 5 residents. The programs are a major source of health coverage for children, pregnant women, seniors with low incomes and people with physical and developmental disabilities.
Medicaid and PeachCare cover about 1.4 million children, or half of all children in Georgia. Medicaid also pays for more than half of all births in Georgia. PeachCare is a separate program serving children from families with incomes above the Medicaid threshold, but who often lack access to employer-sponsored coverage. PeachCare is mostly funded by the federal Children’s Health Insurance Program (CHIP).
Medicaid is the main source of health coverage for Georgians with long-term health care needs, both in nursing homes and in community-based settings. Medicaid is the primary payer for three-fourths of nursing home patients in Georgia. Medicaid also helps pay Medicare premiums for more than 200,000 older Georgians.
Low-Income Medicaid serves children, pregnant women and some parents with very low incomes. The Aged, Blind and Disabled portion of the program serves the elderly and people with a qualifying disability. Most Medicaid enrollees qualify through the low-income program, but most of the spending is for elderly and disabled patients.
Medicaid Program Provides Flexibility to Meet Health Needs
Medicaid is a partnership between the state and federal government, with the federal government paying about 67 percent of the state’s total Medicaid costs. This federal support is beneficial for states when facing emergencies or economic downturns, and the federal government can also provide relief by paying more.
Georgia faced budget cuts due to the COVID-19 pandemic and continues to see more people facing economic hardship and enrolling in Medicaid coverage. In response, the federal government is providing a higher matching rate of 73 percent throughout the public health emergency. This amounted to about $165 million in savings in last year’s budget and will continue to produce savings in the 2022 budget year.
With these savings, Georgia is taking steps to build on the Medicaid program. The state received approval this year to extend postpartum Medicaid coverage to six months after delivery, instead of two months. The $20 million allocated for this extension in 2021 remains in the 2022 budget. The 2022 budget also funds Medicaid reimbursement rate increases for certain providers, including skilled nursing centers, home and community-based service providers and select primary and dental care services.
The 2022 budget also includes $76 million for DCH and the Department of Human Services to implement a partial Medicaid expansion with work requirements and premiums. This program is expected to enroll about 30,000 people in the first year, but is pending approval due to concerns about the work reporting requirements presenting an unreasonable burden on enrollees, especially during the pandemic. Georgia could cover over 500,000 people by putting these funds toward a full Medicaid expansion and taking advantage of $1.4 to $1.9 billion in new federal money available to the 14 states—including Georgia—who have yet to implement a full expansion of Medicaid to adults with low incomes.
Inequities in Health Care Access
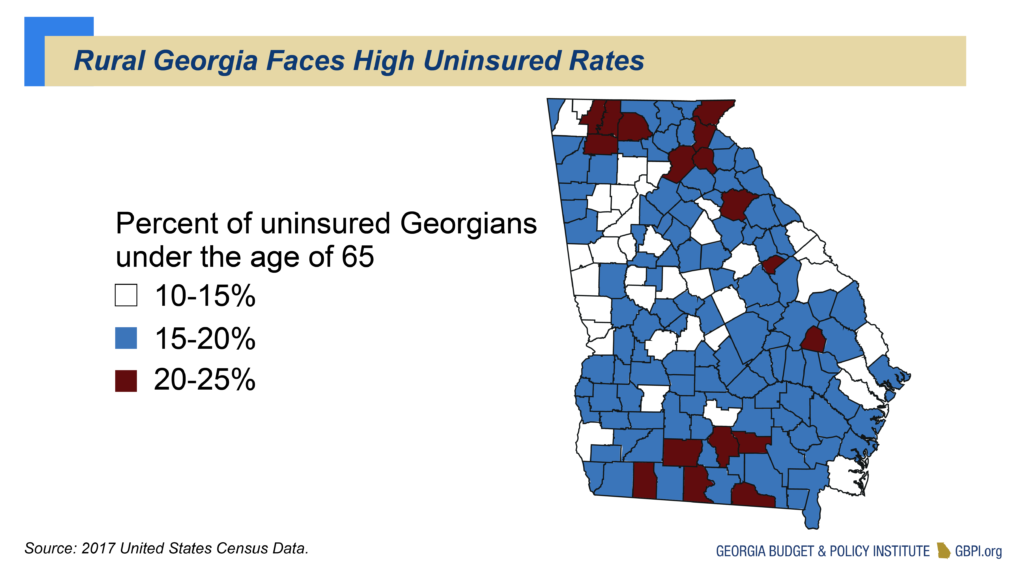
In addition to COVID-19, Georgia faces several health care challenges such as having the third-highest uninsured rate in the nation, rural hospital financial strains, health care worker shortages, rising health care costs and a growing need for mental health and substance use disorder prevention and treatment. Georgia also ranks poorly in several health measures; for example, the state ranks No. 46 for child health, No. 49 for maternal mortality and No. 47 for access to mental health care.
Black and Brown Georgians face worse outcomes for many of these measures. Black women are three to four times more likely to die from pregnancy-related causes. The uninsured rate for Latinx Georgians is over 2.5 times higher than for white Georgians. These differences are the result of structural racism, a collection of discriminatory policies and racial biases across several facets of life (e.g., medical providers underestimate Black patients’ pain) that negatively affect outcomes for people of color. Georgia leaders must treat racism as a public health crisis and pursue solutions to undo these inequities.
Recent state efforts to extend postpartum coverage and streamline enrollment for uninsured children into Medicaid by using Supplemental Nutrition Assistance Program (SNAP) data help address these disparities. Georgia can also increase health care access by expanding Medicaid coverage to more than half a million Georgians, with 90 percent of the costs funded by the federal government. Rural Georgia counties, especially in Southwest Georgia and the area known as the Black Belt where counties have larger Black populations, have higher uninsured rates and faced a higher proportion of COVID-19 cases and deaths. Rural residents and hospitals stand to benefit the most from expansion, but every region of the state would see benefits.
Expanding Medicaid Helps Georgians Beyond Health Care
Access to health care is an essential part of life. Unfortunately, Georgians across our state persistently struggle to gain or afford health coverage, leaving them unable to access the critical care they need, affecting their ability to work and harming their overall livelihood.
Georgia continues to have one of the highest uninsured rates in the nation. Hundreds of thousands of Georgians fall into the coverage gap, which means their incomes are too high to be eligible for Medicaid but below the minimum income eligibility to receive tax credits that help many afford insurance through Healthcare.gov. About 47 percent of Georgians in the coverage gap are Black, and 9 percent are Latinx.
These disparities are exacerbated by Georgia leaders’ refusal to fully expand Medicaid, even though this option would benefit Georgia communities while remaining fiscally responsible. Under the Affordable Care Act, states can expand Medicaid eligibility to people with incomes up to 138 percent of the federal poverty level—roughly $17,774 for an individual. Medicaid expansion would bring billions of dollars in federal aid to our state in order to extend coverage to hundreds of thousands of Georgians, stabilize rural health systems and provide myriad economic benefits.
Medicaid is not only vital to health. This program has a long history of supporting Georgia’s K-12 students. Research shows health coverage has a significant impact on educational achievement and future earnings. In higher education, the student uninsured rate in non-expansion states is nearly double that of states that have adopted full Medicaid expansion. A lack of access to health care can keep students out of classrooms longer and make it difficult to complete classwork.
Medicaid is also a crucial component of our safety net. Research shows links between increased health coverage and the ability to work regularly or search for employment. Expansion can also help lift many Georgia families out of poverty because more families would be able to avoid costly payments for health care services they need. Research shows states participating in Medicaid expansion are more likely to generate increased early access to health insurance, providing opportunities for greater economic mobility from one generation to the next.
Expansion also matters for our state’s criminal legal systems. People who were previously incarcerated in non-Medicaid expansion states like Georgia have the worst chances of getting health coverage and care despite having the highest likelihood of chronic illness. Full expansion can provide a gateway to link incarceration-exiting Georgians to health coverage, which will improve their health, reduce emergency room visits and reduce recidivism because people can access the physical and mental health services they need.
Economic benefits also come with expansion. Medicaid expansion could bring more than 64,000 jobs to Georgia. New federal incentives to encourage states to expand Medicaid would send between $1.4 to $1.9 billion to Georgia. This funding would more than cover the cost of expansion, providing extra dollars to address other state priorities like rural broadband, additional support for K-12 students living in poverty and more.
Medicaid expansion is the clear choice for the health of Georgians, hospitals and our state budget.
Behavioral Health and Developmental Disabilities
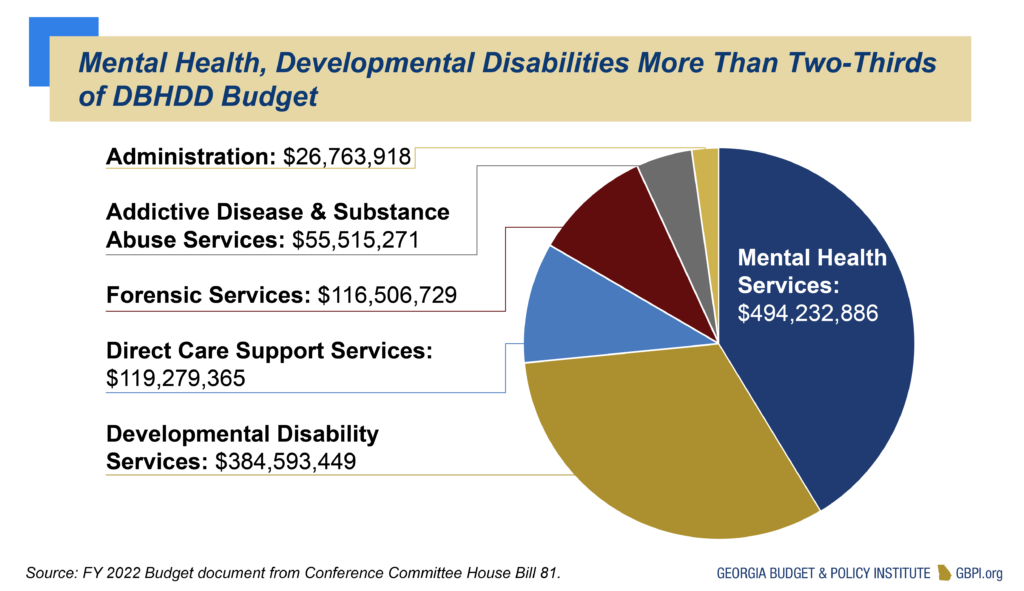
The Department of Behavioral Health and Developmental Disabilities (DBHDD) operates a variety of programs that serve Georgians with mental health needs, substance use disorders and developmental disabilities. The department also operates programs for forensic evaluation and treatment for Georgians under court jurisdiction. DBHDD receives almost $1.2 billion in 2022 from the General Fund along with $10.3 million in Tobacco Funds, a combined increase of $58.9 million compared to 2021. Through the ARP, the agency is also set to receive $45 million in federal block grants funds for community mental health services and $46 million for substance use disorder prevention and treatment to be spent by federal fiscal year 2025.
Georgia entered into a legal settlement in 2010 with the U.S. Department of Justice that laid out a plan for the state to increase its mental health and developmental disability services in home or community settings rather than institutions. The state has invested over $256 million since 2011, including supportive housing for people moving out of institutions, strengthening the behavioral crisis response system and adding new community-based behavioral health services. But the agency faced $91 million in cuts in 2021 and has ongoing needs to address in the settlement.
Public Health
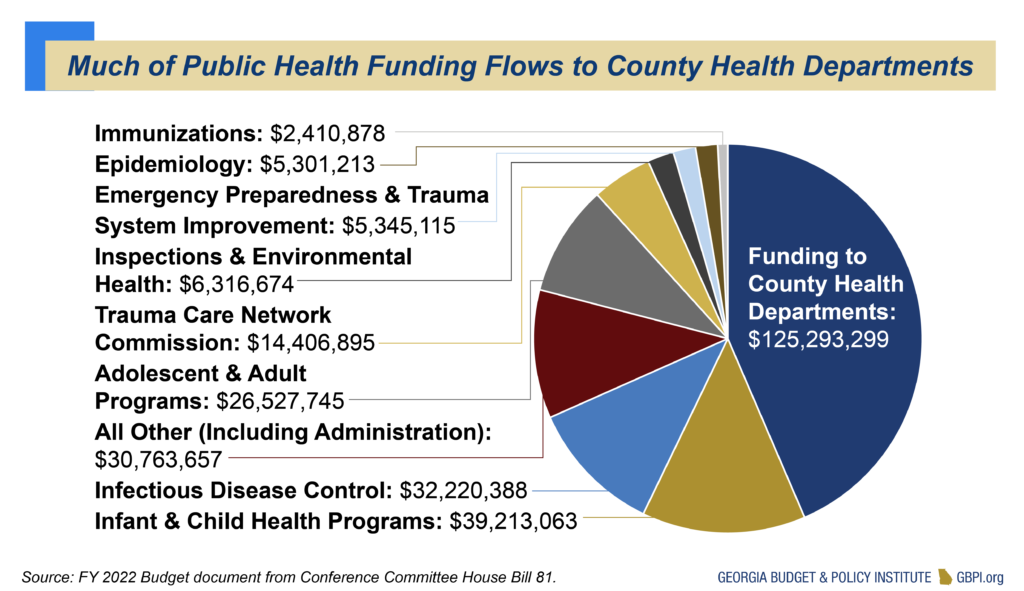
The Department of Public Health operates a variety of programs focused on health promotion, disease prevention and health-related disaster response and preparedness. The department receives $273 million from the General Fund and $13.7 million in Tobacco Settlement money in 2022. The Trauma Care Network Commission, which is included in the department’s budget, receives $14.4 million from the General Fund in 2021. The largest state-funded programs provide financial assistance to county health departments, aim to prevent the spread of infectious disease and provide treatment and health promotion services aimed at children and infants. The department’s 2022 budget increased by $3.8 million compared to 2021.
Georgia’s public health programs also receive significant federal support. Federal money accounts for 57 percent of the department’s $690 million budget in 2022, while state funding accounts for the rest. This does not include additional federal relief for COVID-19. The federally funded Special Supplemental Nutrition Program for Women, Infants and Children, also known as WIC, makes up almost half of the department’s federal funds. Georgia’s WIC program will receive an additional $13.2 million through the ARP, which allows states to increase the amount of the cash-value voucher program that provides participants with money to purchase only fruits and vegetables.
Budget Cuts Remain for Behavioral Health and Public Health
Due to enhanced federal funding in the federal COVID-19 relief packages, the Medicaid agency did not have to make any cuts to eligibility, benefits or reimbursement rates. But the behavioral health and public health agencies did face budget cuts in areas such as mental health services, peer support services, housing vouchers for people with mental illness, funds that would have expanded residential substance use disorder treatment and cuts to health promotion program and trauma center readiness. These funds were partially restored in the 2022 budget.
About $59 million of the $91 million in 2021 budget cuts was restored for the Department of Behavioral Health and Developmental Disabilities. Notable additions include 100 added New Option Waiver Program (NOW) and Comprehensive Support Waiver Program (COMP) slots for home- and community-based services, restoring funds for services for people on the waiver waiting list, increasing reimbursements for intellectual and developmental disability providers, expanding the APEX school-based mental health program and funding to allow about 4,000 more people to get outpatient mental health services and about 3,000 more people to get outpatient substance use disorder services.
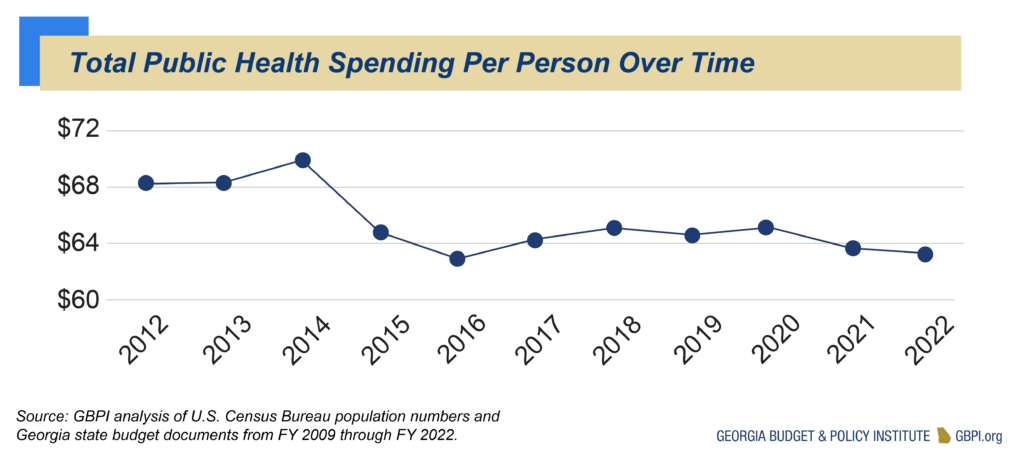
For the Department of Public Health, about $3.8 million of the $8.2 million cut in 2021 have been restored. While the governor’s proposed 2022 budget did not add new money for public health during COVID-19, pointing to new federal money supporting the agency, the House and Senate wanted to provide state dollars to help support the agency as they face ongoing capacity needs and non-COVID-19 related activities. Funds were restored for several health promotion programs, and new money was added for three leadership positions and maintenance for the state’s vaccine management system.
Georgia Health Agencies Respond to COVID-19 Public Health Emergency
Gov. Kemp declared Georgia’s first public health state of emergency on March 14, 2020. DPH and the Georgia Emergency Management Agency (GEMA) are leading the state’s response to the COVID-19 public health emergency and are tasked with preventing the spread of the virus. The amended 2020 budget that passed in March included $100 million from the state’s Revenue Shortfall Reserve to help GEMA and DPH in its COVID-19 response efforts. GEMA also received $54.5 million from the Governor’s Emergency Fund in their work to build treatment and testing capacity and distribute supplies to hospitals and health departments.
DPH aimed to hire nearly 1,000 contact tracers to assist in identifying and mitigating virus hotspots. DPH also responded with additional services such as a COVID-19 Hotline for individuals to access health care if they suspect they are infected, an online monitoring tool and a state data dashboard to track the virus. DPH runs the state’s vaccination management system and supports local health departments in their role to administer vaccines—along with health care facilities, pharmacies and mass vaccination sites.
DCH is also helping with the response through changes to Medicaid. The agency submitted federal waivers to ease health care provider enrollment in Medicaid, expand the use of telehealth services and pause the requirement for current enrollees to renew coverage or pay copayments during the emergency period. The department is also responsible for the oversight of nursing homes and is utilizing existing funds to track COVID-19 cases and deaths and study the impact of COVID-19 on the financial viability of these facilities. The Department of Behavioral Health and Developmental Disabilities (DBHDD) is tracking COVID-19 cases in the state’s five psychiatric hospitals.