In July 2023 Georgia launched the Pathways to Coverage program, which provides a new Medicaid option to uninsured, low-income adults who can report working, going to school, or engaging in other qualifying activities for at least 80 hours per month. The program covers many of the same medical services as traditional Medicaid, including doctor visits, hospital stays and prescriptions. This research brief provides a two-year update on 1) eligibility and enrollment trends, 2) program costs, 3) updates to the program’s design and 4) the potential future impact of a new federal law. The research brief also offers recommendations to state agency staff and state policymakers to make the program more efficient and less costly moving forward.
Here are some key takeaways after two years of program implementation:
- About 8,077 Georgians were actively enrolled in the Pathways to Coverage program by the end of the first two years, which represents no more than 7% of uninsured, low-income adults from working households.
- Failure to meet the qualifying hours and activities reporting requirement prevented about 54% of interested Georgians from even applying and led to about 11% of application denials.
- Too many Georgians were denied coverage for procedural reasons – about 22% of application denials and about 30% of total disenrollments are due to paperwork issues, like a missing document.
- The Pathways to Coverage program cost taxpayers about $110 million, and health care benefits – like doctor visits and prescription refills – accounted for less than $1 in every $3 total dollars spent.
- Georgia has received federal approval to temporarily extend the program through December 2026 and to make changes to who is eligible and how often they must report their qualifying hours and activities.
Section 1: Eligibility and Enrollment Trends
About one in every three of Georgia’s low-income adults is uninsured, and Pathways to Coverage has largely left that reality unchanged.[1]
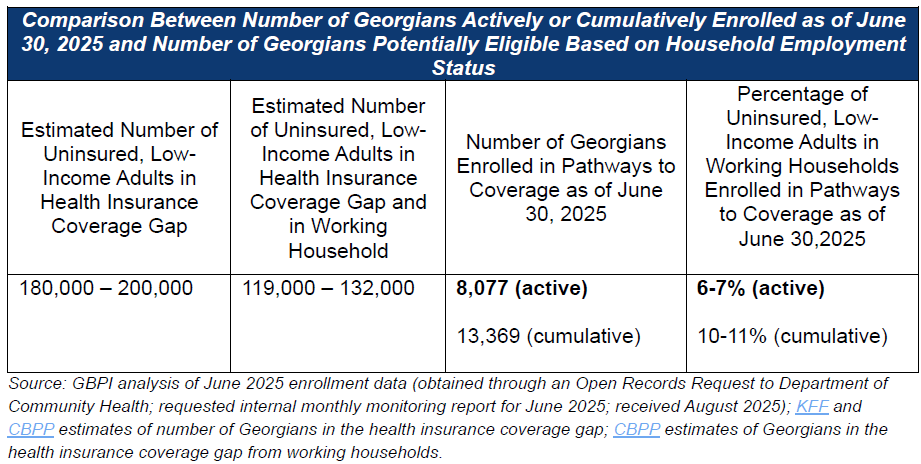
In Georgia, about 240,000 adults aged 19-64 years old who earn less than 100% of the federal poverty level (about $32,000 for a family of four) lack health insurance.[2] Between 180,000 – 200,000 of those Georgians are in the health insurance coverage gap and are U.S. citizens or legally residing non-citizens.[3],[4] Being in the health insurance coverage gap means they are not eligible for traditional Medicaid (i.e., not pregnant/postpartum, not disabled and eligible for SSI, etc.), but they also do not earn enough to qualify for marketplace tax credits. About 66% of Georgians in the health insurance coverage gap are in a family with at least one worker or are working themselves; about 30% are parent caregivers; and about 21% live in a rural county.[5] About 13,369 total Georgians had been enrolled in the Pathways to Coverage program at some point during the first two years, which accounts for cumulative enrollment. Only 8,077 of those Georgians were still actively enrolled in the program by the end of those two years (June 30, 2025), which represents about 6-7% of low-income adults from working households.
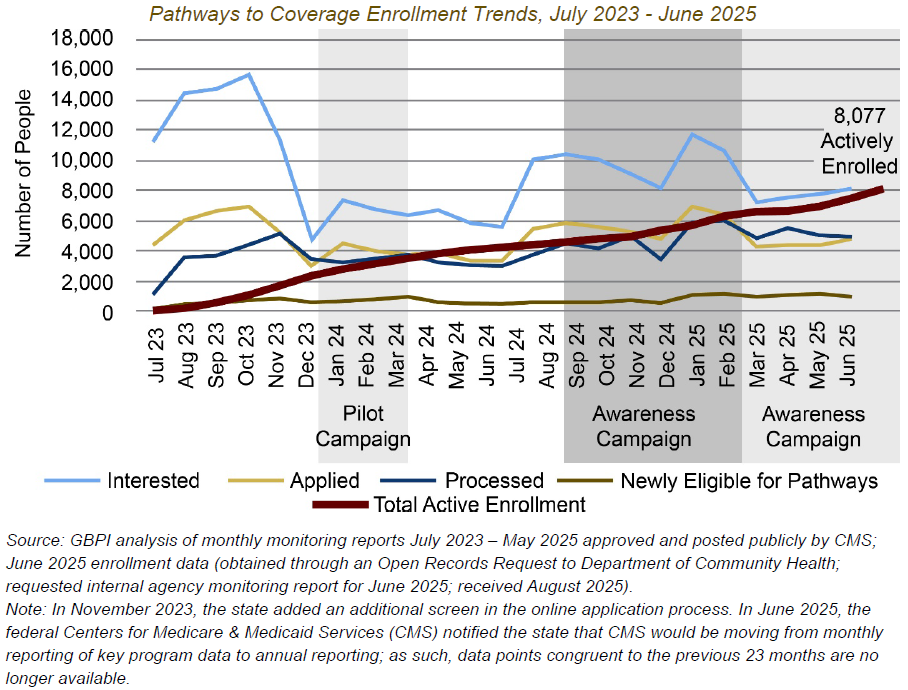
Despite significant and ongoing investment in awareness activities, application volume and active enrollment saw minimal growth between year one and year two.
From January 2024 to March 2024, the state tested a pilot paid media campaign. Leveraging almost $11 million in American Rescue Plan Act (ARPA) funding, the state then expanded into additional marketing and outreach activities from August 2024 to January 2025. Building on the results of those pilots, the state awarded an additional $10 million in federal ARPA dollars to fund a Pathways to Coverage comprehensive awareness campaign from February 2025 to November 2025.[6] The impact of those investments on application submissions and active enrollment is unclear. Monthly application submissions averaged 4,534 in year one and 5,269 in year two, which amounts to about a 16% increase. Although clicks on the ‘Apply Now’ button on the Pathways to Coverage website increased from about 5,000 in February 2025 to almost 45,000 in June 2025, application volume remained consistent in the same time period. Active enrollment at year two (8,077) was less than double what it was in year one (4,231). Since January 2024, monthly growth in active enrollment did not exceed 15%; in year two average monthly growth in active enrollment was just 6%.
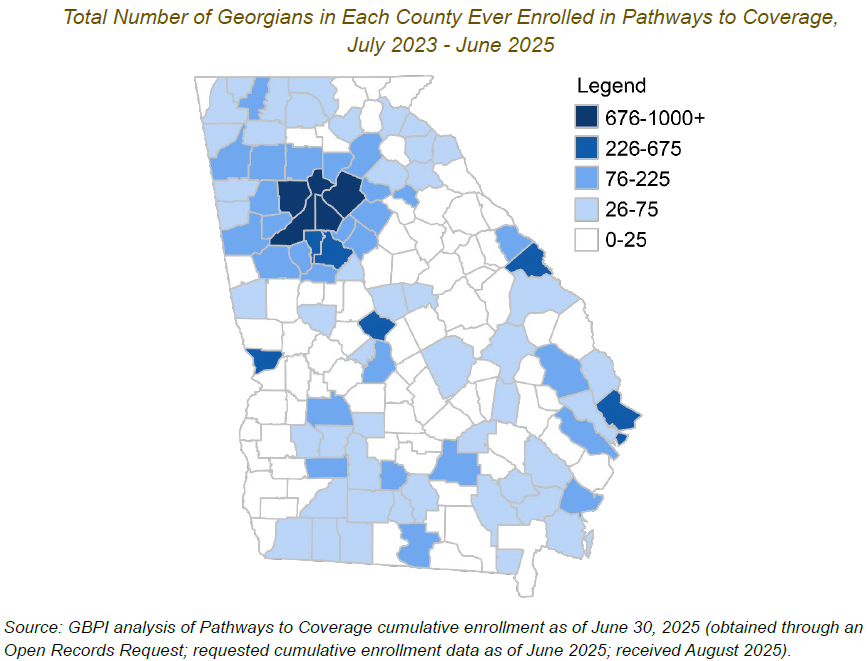
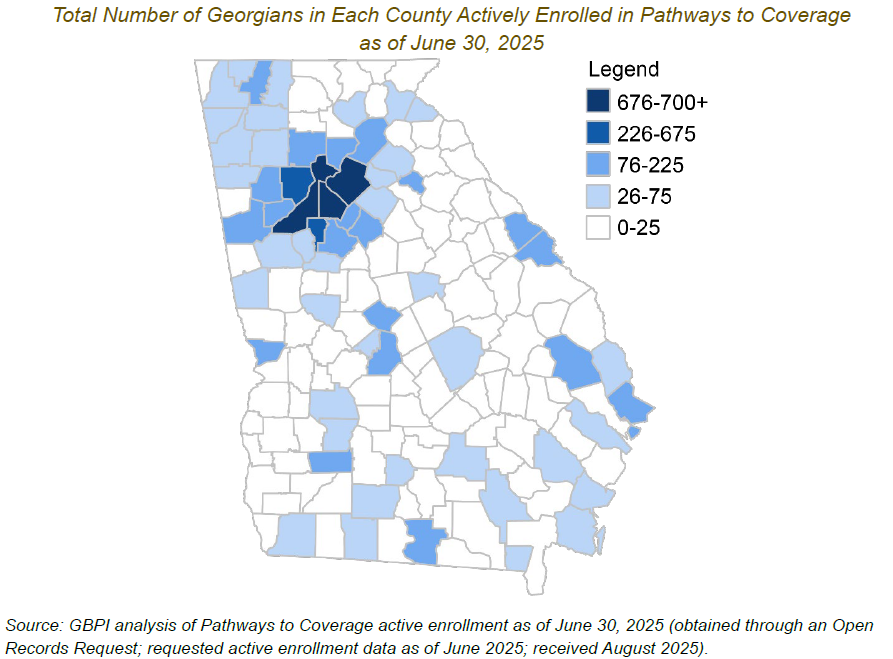
Almost half (48%) of Georgia’s counties still had 25 or fewer residents who had ever been covered under the Pathways to Coverage program after two years of enrollment.
The highest number of residents ever enrolled in the program by county were, as expected, clustered in densely populated counties in metro areas like Atlanta, Augusta and Savannah. Fulton County had the highest number of residents ever enrolled in the program (1,180 residents) while the small, rural southwest counties of Webster and Baker had the lowest number of residents ever enrolled in the program (0 residents). By June 30, 2025, an average of about three in every five people who had gained coverage under the Pathways to Coverage program in each county were still actively enrolled (excludes Webster and Baker counties). For example, about 70% of Clarke County’s enrollees were still actively enrolled as of June 30, 2025, whereas about 54% of the residents in Bibb County who had ever enrolled in the program were still enrolled.
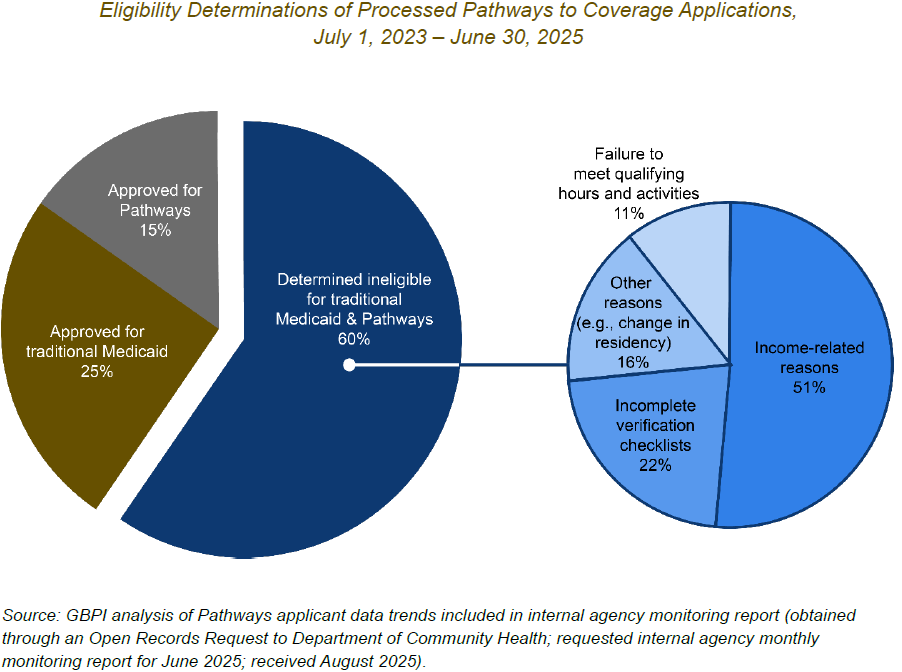
About 60% of Pathways to Coverage applications were denied in the first two years, and failure to meeting the qualifying hours and activities requirement accounted for 11% of those denials.
Of the complete Pathways to Coverage applications processed within the first two years, about 15% were approved for Pathways to Coverage, 25% were approved for traditional Medicaid and the remaining 60% were denied coverage. The reasons for being denied coverage vary. For example, about one in every five application denials was for procedural or ‘paperwork’ issues like failure to provide a copy of a birth certificate or driver’s license.
Notably, about one in every 10 of the application denials was due to failure to meet the qualifying hours and activities requirement. However, that data point does not fully illustrate the impact this reporting requirement has on applicants’ ability to gain coverage. For example, earlier in the application process, after an individual has elected to be considered for Pathways to Coverage and acknowledged that they read the requirements of the program, they must report valid qualifying hours and activities to move on to the next step and be considered as having a complete application. In the first two years, the failure to report a non-zero number of qualifying hours and activities or request a reasonable modification (for individuals with disabilities) prevented about 54% of those who demonstrated interest in applying from submitting a complete application.
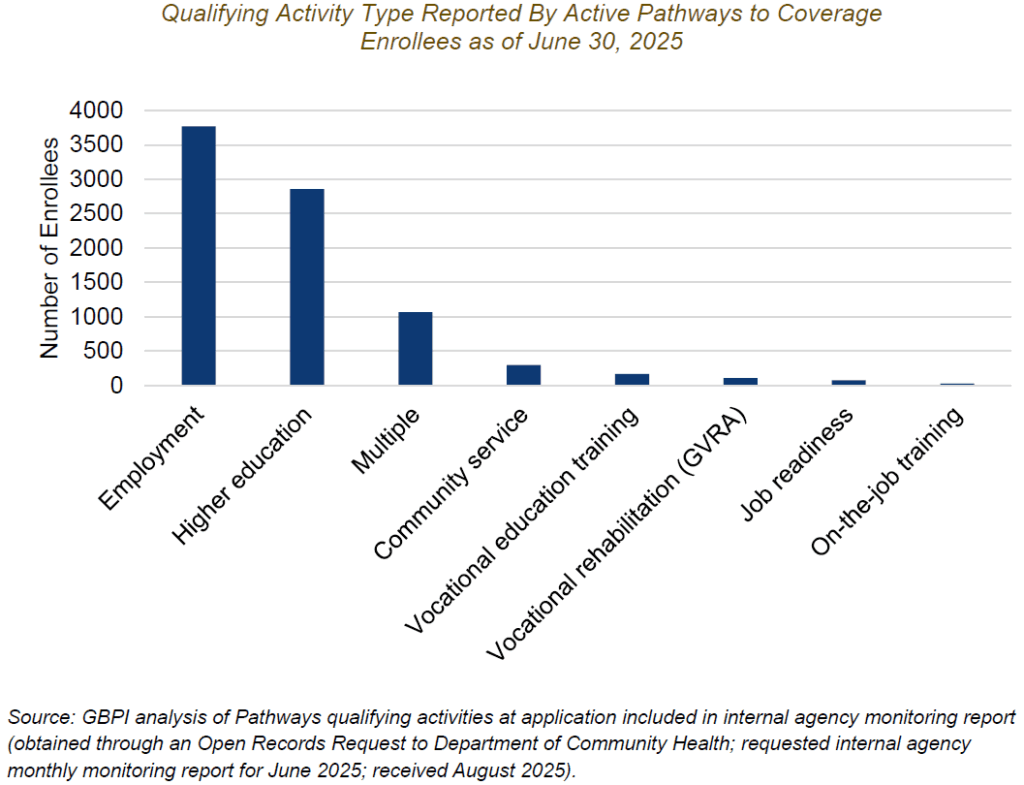
A majority (79%) of active enrollees gained coverage through employment or higher education.
Among the over 8,000 Georgians who were eligible for the Pathways to Coverage program as of the end of June 2025, most qualified under employment (including self-employment) or enrollment in higher education. An additional 13% reported multiple qualifying activities, most of which were a combination of employment and higher education. About 5% qualified under a work program and 4% under community service.
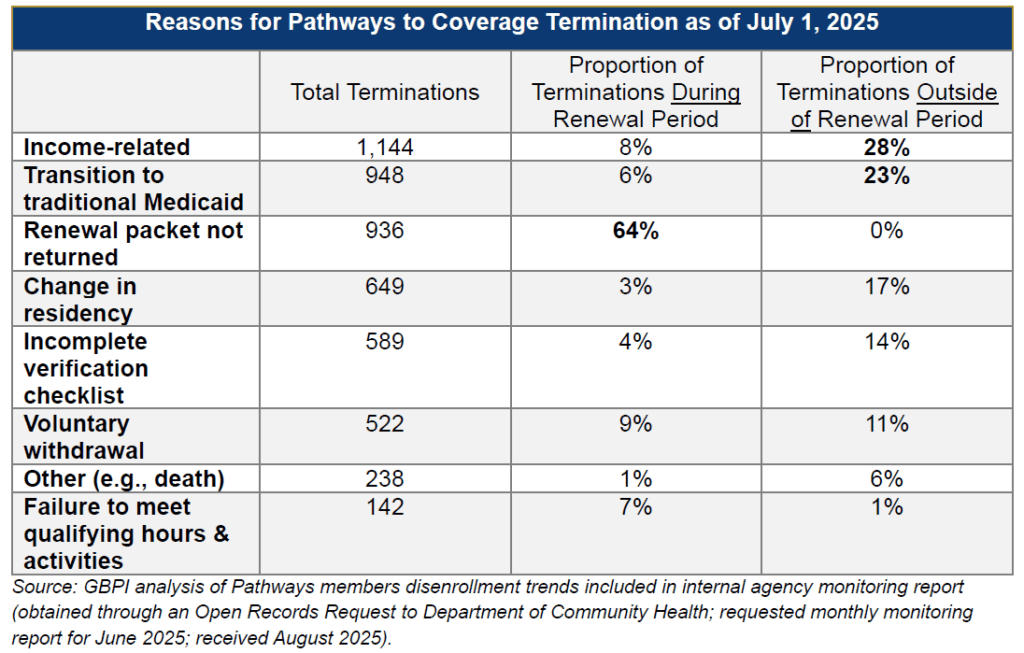
During the renewal period, a majority (64%) of disenrolled Georgians lost coverage because they did not return their renewal packet.
As of July 1, 2025, 5,168 Georgians had been disenrolled and remained disenrolled. Outside of the renewal period, a majority of enrollees who lost coverage lost it for income-related reasons (like household earnings going above 100% of the federal poverty level) or because they transitioned to traditional Medicaid due to pregnancy or another change in eligibility. During the renewal period, most enrollees who lost coverage lost it because they did not return their renewal packet. In total, both during and outside the renewal period, about 30% of enrollees lost their coverage because of ‘paperwork’ reasons like not returning the renewal packet or not providing documents like a birth certificate or driver’s license.
Based on the available data, the program has not meaningfully increased employment or participation in employer-sponsored health coverage.
According to the state, two of the key goals of the Pathways to Coverage program are to promote employment and encourage participation in employer-sponsored health insurance coverage.[7] One study found that, in the first 15 months of the Pathways to Coverage program, there was no change in employment in Georgia compared with neighboring non-expansion states like Florida and South Carolina.[8] Moreover, the Pathways to Coverage Health Insurance Premium Payment program, which covers premiums and other cost-sharing for eligible Georgians covered under their employer’s health insurance plan, had just two enrollees as of June 30, 2025.[9] Prior research demonstrates that work requirements have minimal impact on long-term employment gains.[10],[11] Most people who are in the health insurance coverage gap are already in a family with at least one worker or are working themselves.[12] However, they are often employed in jobs that do not offer employer-sponsored coverage, such as construction, food service and retail.[13] Those who are not working are often caring for children or other family members, living with a serious health condition or disability or are enrolled in school.[14]
Section 2: Program Costs
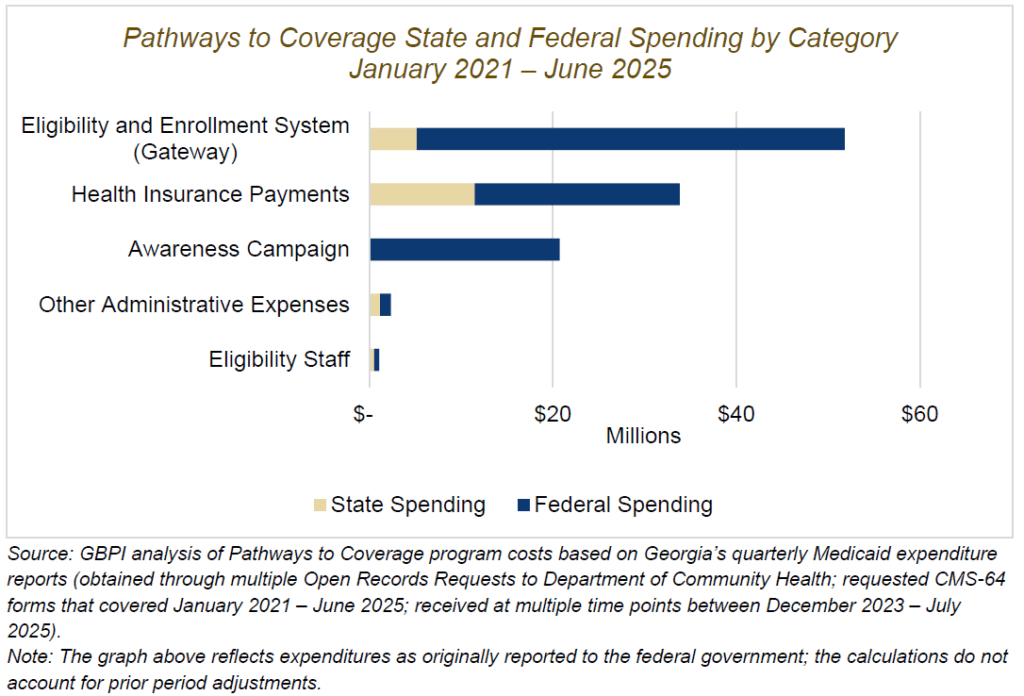
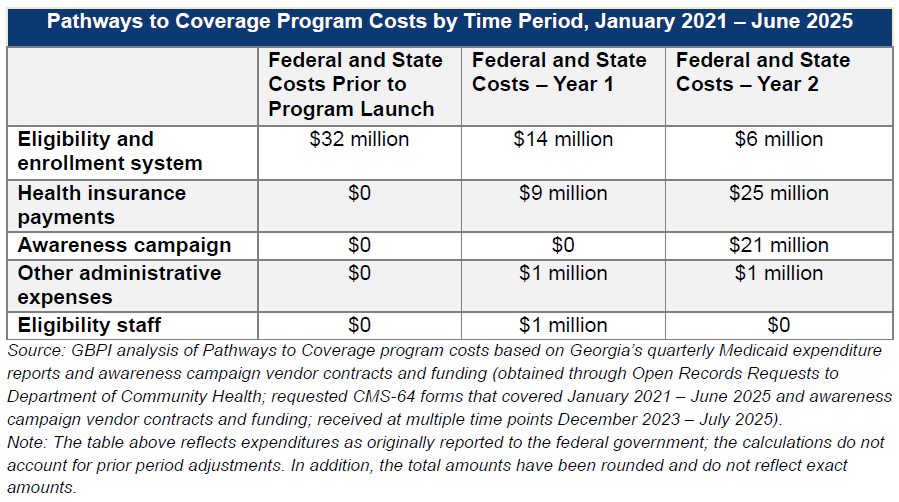
Through June 2025 the Pathways to Coverage program cost taxpayers about $110 million, and health care benefits, like doctor visits and prescription refills, represented less than $1 in every $3 total dollars spent.[15]
Health care benefits accounted for about 31% of total costs from program approval through the end of year two. In that same time period about $52 million was spent on the eligibility and enrollment technology , which accounts for about 47% of total program costs. In year two alone, almost as much was spent on the awareness campaign (almost $21 million in federal American Rescue Plan Act funds) as was spent on health care benefits (almost $25 million in combined state and funds).[16] Overall, Georgia had spent about $13,597 per active enrollee as of June 30, 2025 on total program costs. The combined $110 million does not account for expenses related to preparing and submitting the original 1115 demonstration waiver, expenses related to the two Pathways to Coverage lawsuits filed by the state or funding for a pilot media campaign that ran January 2024 to March 2024.
The federal government has covered about 83% of total program costs, and most federal dollars were spent on upgrades to Georgia’s eligibility and enrollment system, the awareness campaign and other administrative expenses such as those related to program evaluation.[17]
Georgia, like all states, pays about 10 cents on the dollar for designing and installing new functionality in its eligibility and enrollment technology system (known as Gateway), which means the federal government covers most of the cost. Georgia has spent state and federal funds on Pathways to Coverage in 15 federal fiscal quarters from January 2021 through the end of June 2025. All 15 of those fiscal quarters have included Pathways-related upgrades to the eligibility and enrollment technology system. Although the spending on technology upgrades decreased over time, it has been a consistent expense that appears likely to continue.
Section 3: Current Program Changes and Future Impact of New Federal Law
Georgia received federal approval to temporarily extend the program through December 2026 and to make changes to who is eligible and how often they must report their qualifying hours and activities.[18]
Georgia received federal approval to temporarily extend the program through December 31, 2026 (for a more detailed timeline from original program approval in October 2020 to the present, please visit this website). In addition, the state also received federal approval to make program updates (listed below) starting in October 2025. Even with the changes, by October 2026 near the end of the temporary extension, the state estimates that only 18,301 Georgians will be actively enrolled.[19]
- New qualifying activities for parents of young children and food assistance recipients: Caregiving of a child under 6 years old who is currently enrolled in or applying for Medicaid is now a qualifying activity. Another new qualifying activity is compliance with the requirements of the Supplemental Nutrition Assistance Program (SNAP), a program with a similar work reporting requirement that helps low-income households afford the cost of food.
- Annual reporting: Enrollees verify their qualifying hours and activities at initial enrollment and annual renewal rather than on a monthly basis as was the case in the original Pathways program design. Because automatic audits were never implemented, the state did not systematically suspend or terminate coverage in the first two years based on monthly reporting.
- Removal of premiums, tobacco surcharges and modified copayments: Premiums, copayments and incentives, which were originally authorized but never implemented, have been removed. Enrollees are now subject to the same copayments as traditional Medicaid enrollees.
- Modified coverage start date: Enrollees now start coverage the first day of the month in which the application was submitted rather than the first day of the month after eligibility was determined as was previously the case.
Relative caregiving, outside of parenting a child under the age of 6, and a stay in a skilled nursing facility or hospital were already qualifying activities but have been newly added to the program’s website.[20]
The state updated its program website in October 2025 and now specifically lists caregiving for a relative as a qualifying activity. To be eligible, the caregiver must be a paid caregiver for a relative enrolled in one of the state’s Medicaid waiver programs for older adults or individuals with disabilities. As of June 2025, about 21% of those whose qualifying activity was community service specifically reported caregiving of a relative as their community service. Similarly, though it was already an allowable activity, a stay in a skilled nursing facility/hospital has also been newly listed on the program website as a qualifying activity.
The state has implemented or planned systems-level updates to improve the application process and ease the administrative burden on applicants, enrollees and frontline caseworkers.
Going forward, the state will be re-procuring and replacing the technology system used for eligibility and enrollment processing (currently known as Gateway).[21],[22] In the meantime, the state is making tweaks to the existing system. For example, in March 2025, the state began sending text message reminders to Pathways to Coverage applicants who had missing information. That same month, the state updated the application status tracker on Gateway (the eligibility and enrollment technology system) to help applicants better understand where they stand in the eligibility determination process. In July 2025, the state launched a mobile responsive Gateway portal to allow Georgians to apply for public benefits like Medicaid more easily on their mobile device and added a specific ‘Apply for Pathways’ option to the Gateway homepage. Below are some additional changes under development that may reduce bureaucratic red tape and make the application process more human-centered.
- Simplifying language on all Pathways-related Gateway screens and in written notices to increase understanding of information
- Removing the Pathways to Coverage contract signature requirement and using the existing Medicaid application signature instead
- Reducing the number of Pathways screens at the end of the Medicaid application from four to two
Notably, many of these changes to Gateway are system-wide and thus the state can report the costs associated with these changes as administrative expenses for the state’s overall Medicaid program.[23]
Starting in January 2027, Georgia will likely need to align more closely with the work and other qualifying activities reporting requirement created under the 2025 H.R. 1 budget reconciliation law.
In its extension application, the state requested federal approval to run the Pathways to Coverage program through 2030.[24] However, the Centers for Medicare & Medicaid Services (CMS) provided only a temporary extension through December 31, 2026. The approval specifically cites H.R. 1 (formerly known as the One Big Beautiful Bill Act, or OBBBA) and the need to comply with the new federal provisions related to a Medicaid work and other qualifying activities requirement that goes into effect after December 31, 2026. [25]
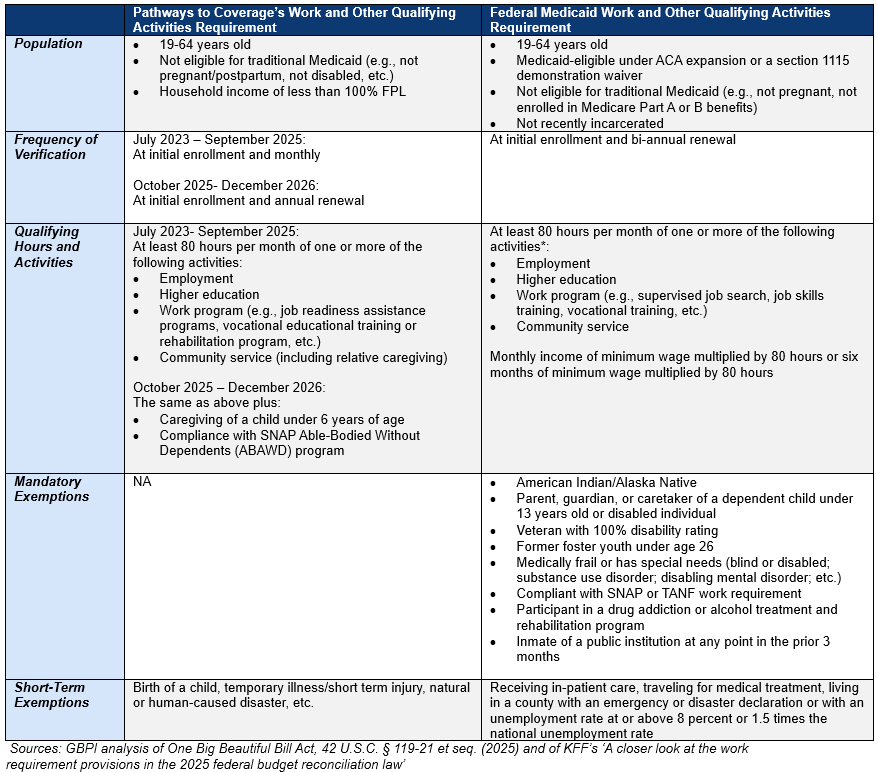
The Pathways to Coverage work and other qualifying activities reporting requirement has more restrictive criteria, but less frequent eligibility checks compared to the requirement created under the 2025 H.R. 1 budget reconciliation law.[26],[27]
Even with the program updates, Pathways to Coverage does not include any long-term reporting exemptions. For example, the H.R. 1 provisions exempt groups like former foster youth under the age of 26, fully disabled Veterans and medically frail individuals from having to report work and other qualifying activities in order to qualify for Medicaid. Similarly, Pathways to Coverage makes caregiving of children younger than 6 years old a qualifying activity, whereas caregiving of children younger than 13 or of a disabled individual is an exemption under H.R. 1. On the other hand, Pathways to Coverage enrollees only have to re-verify their qualifying hours and activities at annual renewal while the new federal law requires bi-annual eligibility checks. For a detailed comparison chart, see Appendix.
Section 4. Recommendations
Both now and when the temporary program extension expires in December 2026, the state has an opportunity to leverage lessons learned to make the program more inclusive and less administratively burdensome for eligible Georgians and less costly for taxpayers. As policymakers, state agency leadership and advocates consider options moving forward, GBPI offers the following recommendations.
Short-term: Programmatic enhancements
Prior to the expiration of the temporary program extension in December 2026, the state should consider minor programmatic augmentations to raise awareness of the October 2025 program changes and maximize enrollment among eligible Georgians. Two examples are listed below:
- Provide virtual trainings on program updates for community-based enrollment assisters, relevant staff at care management organizations and others who provide direct services to uninsured low-income Georgians. The state could provide a series of virtual trainings to relevant ‘helpers’ to raise awareness of the October 2025 program changes, like the new qualifying activities and change to annual reporting, and systems changes like the text message reminders for applicants with missing paperwork. The training could also provide guidance on how to assist newly eligible Georgians with documenting the new qualifying activities.
- Use existing data to automatically process the eligibility of parents of Medicaid-enrolled young children and individuals who are currently SNAP compliant. Rather than waiting for them to learn about the program and submit a new application, the state could use existing data to proactively process the eligibility of parents of Medicaid-enrolled children under the age of 6 and of individuals compliant with SNAP’s work requirement. Those deemed eligible for the Pathways to Coverage program could be notified and then either choose to enroll or opt out. Prior research shows that increasing the use of electronic data sources to verify eligibility can reduce the burden on applicants/enrollees and on the frontline caseworkers processing their applications as well as potentially reducing overall costs to the state.[28]
Medium-term: Programmatic evolution
After the expiration of the temporary program extension in December 2026, the state should consider more comprehensive changes that make program eligibility less restrictive and decrease the state’s per-person cost. Two examples are listed below:
- Align with the qualifying activities and reporting exemptions as written in the 2025 federal budget reconciliation law H.R. 1. In the extension approval letter, CMS states that Georgia must comply with and implement the new work and other qualifying activities reporting requirement as written in H.R. 1. Greater alignment with the federally mandated work and other qualifying activities reporting requirement could expand eligibility for more Georgians. For example, the state could include reporting exemptions for former foster youth under the age of 26, fully disabled Veterans, medically frail individuals, parents of children under the age of 13 and people living in counties with high unemployment rates.
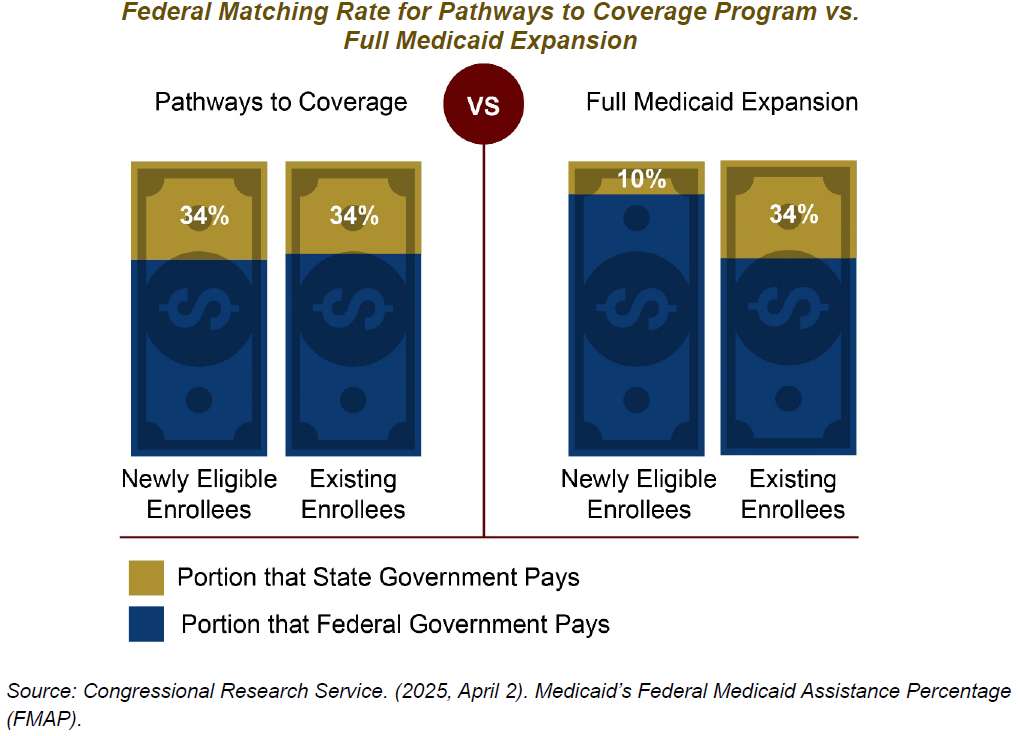
- Raise the Medicaid income eligibility limit for non-elderly, non-pregnant adults up to 138% of the federal poverty level. By January 2027, forty other states plus DC will join Georgia in implementing a Medicaid work and other qualifying activities requirement for low-income adults. However, Georgia will be the only state of those 40 paying significantly more per enrollee in state costs. Currently, the state pays about 34% of health care costs for Georgians covered under both traditional Medicaid and the Pathways to Coverage program. If the state expands access to health care for Georgians with annual household incomes of up to 138% of the federal poverty level, the state would cover only 10% of the health care coverage costs for low-income adults as authorized under the Affordable Care Act. Once the temporary extension for the Pathways to Coverage 1115 demonstration waiver ends on December 31, 2026, Georgia could submit a state plan amendment that would allow Georgia to pay less per enrollee in state costs for health care benefits.
Ongoing: Modernization of the eligibility and enrollment infrastructure
As previously recommended by GBPI in a prior report, the state could continue its efforts to transition to a more human-centered eligibility and enrollment system and build up a frontline eligibility workforce that is equitably paid, well-trained and co-located in the communities they serve.[29] Three examples are listed below:
- Add visual examples of verifying documentation to the program website and to Gateway. For example, a stay in a skilled nursing facility or hospital is considered an allowable activity under the job readiness category. However, the only guidance provided on verifying that qualifying activity is vague ( “signed statement from habilitation/rehabilitation institution verifying hours in last four weeks”).[30] The state could add to the program website and to Gateway specific visual examples of acceptable documentation for each qualifying activity.
- Expand automation using reliable data sources and enhance real-time support for applicants and enrollees. Twenty-two percent of Pathways to Coverage application denials and 30% of disenrollments are due to procedural issues like missing paperwork. Decreasing procedural denials and disenrollments requires both technological and human solutions. In November 2025 the state is rolling out a change to Gateway that enables the system to make a real-time eligibility determination without requiring additional information from the applicant. The state could continue this move toward greater automation and use more comprehensive federal and state data sources to accurately verify applicant and enrollee information.[31] At the same time, the state could also improve support for applicants and enrollees that helps minimize confusion and human error. For example, the state could implement a live chat function that is available both during the application and yearly renewal process.
- Ensure the eligibility and enrollment frontline workforce is fully staffed and well compensated. The heavy workload faced by frontline caseworkers contributes to the flawed eligibility and enrollment infrastructure.[32] Retaining trained and experienced frontline staff is critical to ensure that applicants/enrollees are supported and processing is timely.[33] The state could increase staffing levels and adjust salaries to be more competitive.[34]
Ongoing: Improved awareness and outreach among potentially eligible Georgians
As previously recommended by GBPI in a prior report, the state could continue its efforts to raise awareness of the program among potentially eligible Georgians and those who serve them.[35] Two examples are listed below:
- Increase awareness and outreach activities specifically tailored to older adults, rural residents, men and people of Hispanic/Latino ethnicity. According to the interim evaluation by Public Consulting Group, most eligible applicants in the first year were young (19-34 years old), female, and living in an urban area.[36] This indicates that key groups within the low-income uninsured population may not have sufficient information or support to apply for the Pathways to Coverage program. For example, men comprise about 51% of uninsured, low-income Georgians, but only 26% of Pathways-eligible applicants during July 2023 – July 2024. Similarly, Georgians of Hispanic/Latino ethnicity make up about 15% of low-income, uninsured Georgians, but only about 3% of Pathways-eligible applicants during that same time period.[37],[38] The state could explore additional solutions for engaging older adults (50-64 years old), rural residents, men and people of Hispanic/Latino ethnicity.
- Provide mini-grants to community-based organizations that can provide localized and culturally appropriate education and outreach, and where possible, assist with the application process. When working to reach potentially eligible but uninsured populations, best practices emphasize the importance of grassroots outreach, including partnering with trusted community organizations, going where people feel most comfortable and prioritizing in-person interaction.[39],[40] Moreover, community-based organizations can help remove structural barriers that potentially eligible Georgians encounter during the application process. For example, they can provide transportation to the local DFCS office, provide the computer or internet access needed to submit their application or help an individual with low digital literacy upload their verifying documentation. The state could initiate a mini-grant program for trusted messengers and community-based organizations, similar to the mini-grant program launched during the Medicaid unwinding, to assist with raising awareness and providing direct support.[41]
Appendix.
Comparison Between Pathways to Coverage and New Federal Law: Work and Other Qualifying Activities Requirement
Endnotes
Important note on citations: Unless otherwise cited in the list below or in the ‘Source’ section under each table and graph, the findings in this research brief are based on analysis of the Georgia Department of Community Health’s July 2025 internal monitoring report dated July 15, 2025. That report included both monthly monitoring data representing June 2025 and summary data representing July 2023 – June 2025 (e.g., Pathways program status; system enhancement implementation; marketing and outreach campaign; etc.). It was obtained through an Open Records Request and received by GBPI in August 2025.
[1] GBPI analysis of U.S. Census Bureau. “Health Insurance Coverage Status by Ratio of Income to Poverty Level in the Past 12 Months By Age,” American Community Survey 1-Year Estimates, 2024. Retrieved September 15, 2025, from https://data.census.gov/table
[2] Thomas, G. (2024, September 5). Georgia Pathways to Coverage [PowerPoint slides]. Georgia Department of Community Health. https://dch.georgia.gov/document/document/comprehensive-health-coverage-meeting-slide-deckdch-presentation-002/download
[3] Cervantes, S., Bell, C., Tolbert, J., & Damico, A. (2025, February 25). How many uninsured are in the coverage gap and how many could be eligible if all states adopted the Medicaid expansion? KFF. https://www.kff.org/medicaid/how-many-uninsured-are-in-the-coverage-gap-and-how-many-could-be-eligible-if-all-states-adopted-the-medicaid-expansion/
[4] Zhang, E., (2025, April 10). Research note: Closing Medicaid coverage gap would provide 1.5 million uninsured adults path to affordable health coverage. Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/closing-medicaid-coverage-gap-would-provide-over-15-million-uninsured-adults-path
[5] GBPI analysis of Zhang, E., (2025, April 10). Research note: Closing Medicaid coverage gap would provide 1.5 million uninsured adults path to affordable health coverage. Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/closing-medicaid-coverage-gap-would-provide-over-15-million-uninsured-adults-path
[6] Georgia Department of Community Health. Pathways to Coverage awareness campaign vendor contracts and funding. (Obtained through an Open Records Request; requested vendor contracts and funding; received July 2025).
[7] Georgia Department of Community Health. (2025, April 28). Georgia Section 1115 demonstration waiver extension request. https://www.medicaid.gov/medicaid/section-1115-demonstrations/downloads/ga-pathway-pa-04282025.pdf
[8] Johnson, D.Y., Mein, S.A., Marinacci, L.X., Liu, M., & Wadhera, R. (2025). Insurance coverage and employment after Medicaid expansion with work requirements: Quasi-experimental difference-in-differences study. BMJ, 390. https://pubmed.ncbi.nlm.nih.gov/41027709/
[9] Department of Community Health. Cumulative enrollment in the Pathways to Coverage Health Insurance Premium Payment (HIPP) program option. (Obtained through an Open Records Request; requested cumulative enrollment in the Pathways to Coverage Health Insurance Premium Payment program from January 1 2024 – June 30, 2025; received October 2025).
[10] Pavetti, L., Bolen, E., Harker, L., Orris, A., & Mazzara, A. (2023). Expanding work requirements would make it harder for people to meet basic needs. Center on Budget and Policy Priorities. https://www.cbpp.org/research/poverty-and-inequality/expanding-work-requirements-would-make-it-harder-for-people-to-meet
[11] Gangopadhyaya, A. & Karpman, M. (2025, April 9). The impact of Arkansas Medicaid work requirements on coverage and employment: Estimating effects using National Survey Data. Health Services Research. https://doi.org/10.1111/1475-6773.14624
[12] Zhang, E., (2025, April 10). Research note: Closing Medicaid coverage gap would provide 1.5 million uninsured adults path to affordable health coverage. Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/closing-medicaid-coverage-gap-would-provide-over-15-million-uninsured-adults-path
[13] Cervantes, S, Bell, C., Tolbert, J., & Damico, A. (2025, February 25). How many uninsured are in the coverage gap and how many could be eligible if all states adopted the Medicaid expansion? KFF. https://www.kff.org/medicaid/issue-brief/how-many-uninsured-are-in-the-coverage-gap-and-how-many-could-be-eligible-if-all-states-adopted-the-medicaid-expansion/
[14] Rosenbaum, S., Cohen, M., Tavares, J.L., & Barkoff, A. (2025, April 30). Who’s affected by Medicaid work requirements? It’s not who you think. Milbank Quarterly Opinion. https://www.milbank.org/quarterly/opinions/whos-affected-by-medicaid-work-requirements-its-not-who-you-think/
[15] GBPI analysis of Pathways to Coverage program costs based on Georgia’s quarterly Medicaid expenditure reports (Obtained through Open Records Requests to Department of Community Health; requested CMS-64 forms that covered January 2021 – June 2025; received at multiple time points December 2023 – July 2025).
[16] Georgia Department of Community Health. Pathways to Coverage awareness campaign vendor contracts and funding. (Obtained through an Open Records Request; requested vendor contracts and funding; received July 2025).
[17] GBPI analysis of Pathways to Coverage program costs based on Georgia’s quarterly Medicaid expenditure reports (Obtained through Open Records Requests to Department of Community Health; requested CMS-64 forms that covered January 2021 – June 2025; received at multiple time points December 2023 – July 2025).
[18] U.S. Department of Health and Human Services. (2025, September 23). CMS temporary extension approval. https://www.medicaid.gov/medicaid/section-1115-demonstrations/downloads/ga-pathway-to-covrg-cms-tmpry-extn-aprvl-09232025.pdf
[19] Georgia Department of Community Health. (2025, April 28). Georgia Section 1115 demonstration waiver extension request. https://www.medicaid.gov/medicaid/section-1115-demonstrations/downloads/ga-pathway-pa-04282025.pdf
[20] Georgia Department of Community Health. Eligibility criteria. Georgia Pathways to Coverage. https://pathways.georgia.gov/eligibility
[21] Georgia Health Initiative. (2025). Insights on Medicaid in Georgia: Data and trend analyses. https://georgiahealthinitiative.org/wp-content/uploads/2025/01/Insights-on-Medicaid-in-Georgia_Data-Trend-Analyses-January-2025-2.pdf
[22] Chan, L. (2025, June 30). Georgia health primer for state fiscal year 2026. Georgia Budget and Policy Institute. https://gbpi.org/georgia-health-primer-for-state-fiscal-year-2026/
[23] U.S., Government Accountability Office. (2025, September 3). Medicaid demonstrations: Information on administrative spending for Georgia work requirements. https://www.gao.gov/products/gao-25-108160
[24] Georgia Department of Community Health. (2025, April 28). Georgia Section 1115 demonstration waiver extension request. https://www.medicaid.gov/medicaid/section-1115-demonstrations/downloads/ga-pathway-pa-04282025.pdf
[25] U.S. Department of Health and Human Services. (2025, September 23). CMS temporary extension approval. https://www.medicaid.gov/medicaid/section-1115-demonstrations/downloads/ga-pathway-to-covrg-cms-tmpry-extn-aprvl-09232025.pdf
[26] GBPI analysis of One Big Beautiful Bill Act, 42 U.S.C. § 119-21 et seq. (2025).
[27] Hinton, E., Diana, A., & Rudowitz, R. (2025, July 30). A closer look at the work requirement provisions in the 2025 federal budget reconciliation law. KFF. https://www.kff.org/medicaid/a-closer-look-at-the-work-requirement-provisions-in-the-2025-federal-budget-reconciliation-law/
[28] Medicaid and CHIP Payment and Access Commission. (2023). Increasing the rate of ex parte renewals. https://www.macpac.gov/wp-content/uploads/2023/09/Increasing-the-Rate-of-Ex-Parte-Renewals-Brief.pdf
[29] Chan, L. (2025, October 29). Georgia’s Pathways to Coverage program: The first year in review. Georgia Budget and Policy Institute. https://gbpi.org/georgias-pathways-to-coverage-program-the-first-year-in-review/
[30] Georgia Department of Community Health. Report your qualifying activities. Georgia Pathways to Coverage.
[31] Medicaid and CHIP Learning Collaboratives. (2019). Medicaid & CHIP MAGI application processing: Ensuring timely and accurate eligibility determinations [PowerPoint slides]. Centers for Medicare and Medicaid Services. https://www.medicaid.gov/state-resource-center/downloads/mac-learning-collaboratives/timely-accurate-eligibility.pdf
[32] Lucas, L. (2025, April 1). Legislation could require plan to address backlog of federal benefit cases in Georgia. 11 Alive. https://www.11alive.com/article/news/state/georgia-lawmakers-legislation-provision-to-address-medicaid-snap-tanf-benefits-backlog/85-df10c637-cc89-4ed4-adda-f4165e404ec7
[33] Medicaid and CHIP Learning Collaboratives. (2019). Medicaid & CHIP MAGI application processing: Ensuring timely and accurate eligibility determinations [PowerPoint slides]. Centers for Medicare and Medicaid Services. https://www.medicaid.gov/state-resource-center/downloads/mac-learning-collaboratives/timely-accurate-eligibility.pdf
[34] Georgia Department of Human Services.(2025, June 1). 2025 backlog reduction plan. https://www.documentcloud.org/documents/25960128-2025-backlog-reduction-plan-copy/
[35] Chan, L. (2025, October 29). Georgia’s Pathways to Coverage program: The first year in review. Georgia Budget and Policy Institute. https://gbpi.org/georgias-pathways-to-coverage-program-the-first-year-in-review/
[36] Public Consulting Group. (2024, December 16). Georgia Pathways demonstration program interim evaluation report. (Obtained through an Open Records Request; requested interim evaluation report prepared by Public Consulting Group; received January 2025).
[37] Ibid.
[38] Zhang, E., (2025, April 10). Research note: Closing Medicaid coverage gap would provide 1.5 million uninsured adults path to affordable health coverage. Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/closing-medicaid-coverage-gap-would-provide-over-15-million-uninsured-adults-path
[39] Artiga, S., Rudowitz, R., & Tolbert, J. (2016). Outreach and enrollment strategies for reaching the Medicaid eligible but uninsured population. KFF. https://www.kff.org/medicaid/issue-brief/outreach-and-enrollment-strategies-for-reaching-the-medicaid-eligible-but-uninsured-population/
[40] Greene, J., Gibson, D., Quincy, L. & Rappaport, J. (XX). A guide to monitoring Medicaid using lived experience. Center on Budget and Policy Priorities. https://www.cbpp.org/sites/default/files/Monitoring%20Medicaid%20Lived%20Experience%20Report.pdf
[41] Georgia Department of Community Health. DHS and HOPE for Georgia Moms announce community mini-grants [Press release]. https://dch.georgia.gov/announcement/2024-02-08/dhs-and-hope-georgia-moms-announce-community-mini-grants




