Updated February 1, 2023: On December 29, 2022, the Consolidated Appropriations Act of 2023 was signed into law. This law had various implications for the Medicaid unwinding, including de-linking the Medicaid unwinding from the COVID-related public health emergency (PHE) and establishing a more gradual decrease in the enhanced Federal match.
Since the start of the pandemic-era Medicaid continuous coverage requirement, Medicaid enrollment has grown substantially, and over two million Georgians have had uninterrupted access to affordable health care coverage. The Medicaid continuous coverage requirement will begin unwinding on April 1, 2023, and hundreds of thousands of Georgians risk losing coverage. Because they make up 69% of Medicaid and PeachCare beneficiaries in Georgia, children will be disproportionately impacted by losses in coverage. Georgia, like all states, will be facing a massive volume of redeterminations that need to be completed within a 14-month period, which increases the risk that eligible individuals will be erroneously determined ineligible or lose coverage for avoidable procedural reasons (for example, the renewal form is sent to the wrong address). Additional action is needed to avoid unnecessary losses in health care coverage for those who remain eligible and to ensure a smooth transition to other forms of coverage for those who lose eligibility.
By the Numbers
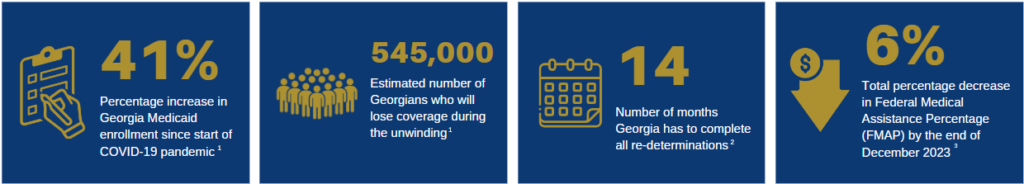
Sources: 1. September 2022 State Audit Report; 2. Centers for Medicare and Medicaid Services; 3. Consolidated Appropriations Act, 2023: Medicaid and CHIP Provisions Explained
Thousands of Georgians are at risk of losing Medicaid coverage once the COVID-related public health emergency ends
The number of Medicaid beneficiaries in Georgia will significantly decline after the PHE expires. The federal government estimates that about 45% of those who lose Medicaid coverage will lose it for procedural reasons—in other words, they lose coverage even though they are still eligible. Though many end up regaining coverage, people who experience this churn often have a harmful gap in access to health care and, among other outcomes, are more likely to delay care, refill prescriptions less often and have more emergency departments visits.
Black and Latinx children are most likely to be impacted
Children overall, who represent about 69 percent of all Medicaid and PeachCare enrollment in Georgia, are at risk for unnecessary losses in coverage. Black and Latinx children, in particular, are overrepresented in Georgia’s Medicaid programs due to inequitable access to economic security brought by a history of racist policies like residential segregation and regressive tax policies. Prior to the pandemic, about 47 percent of Black children and 42 percent of Hispanic children were enrolled in Medicaid and PeachCare compared with about 20 percent of white children.1
Opportunities exist to minimize unnecessary coverage loss and ensure a smooth transition
As documented in the state auditor’s report, the Department of Community Health (DCH) and Department of Human Services (DHS) have taken a proactive approach to communicating with beneficiaries and planning for the end of the PHE. However, there are gaps in the planning that urgently need to be addressed. For example, how does the current Medicaid unwinding plan center the needs and experiences of those who will be most disproportionately impacted? And, what meaningful actions will be taken to help those no longer eligible for Medicaid transition to other forms of coverage?
Listed in the table below are potential state agency and legislative options that may help further mitigate the harm of the Medicaid unwinding.
| Ensuring Eligible Beneficiaries Stay Covered | Improving Transitions to Other Forms of Coverage | Promoting Transparency | |
| Potential state agency options (DCH and DHS) |
|
|
|
| Potential legislative options |
|
|
a. The federal Consolidated Appropriations Act of 2023 requires all states, including Georgia, to implement 12-month continuous Medicaid and PeachCare eligibility for children starting in January 2024. However, Georgia can implement this option more quickly to help children stayed covered during the unwinding.
[1] Based on GBPI analysis of: State Health Access Data Assistance Center (n.d.) 2019 Health Insurance Coverage Type by Race/Ethnicity. [Data set]. Retrieved May 5, 2022, from http://statehealthcompare.shadac.org