State Plans to Launch Two New, State-Run Health Care Programs While Unwinding Medicaid Continuous Coverage
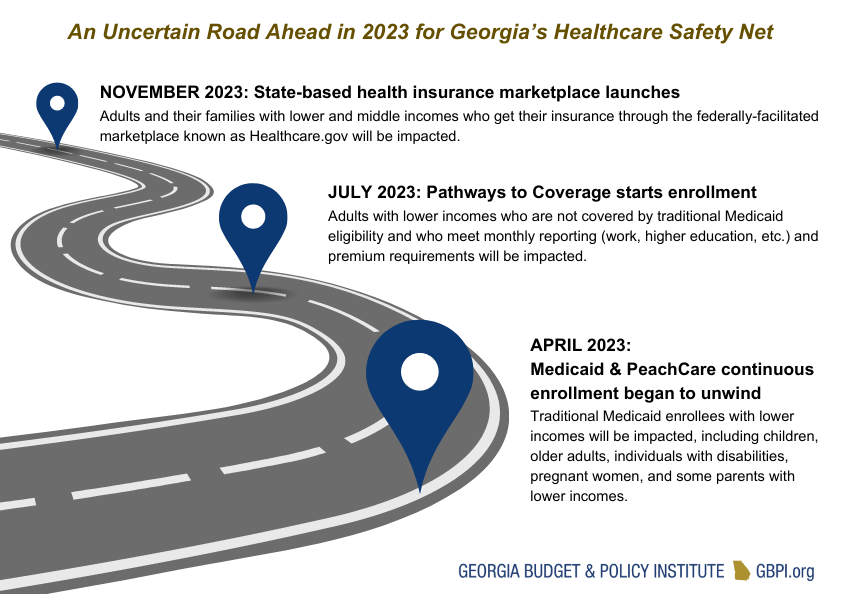
In April 2023, the state began the 14-month process to redetermine the eligibility of all 2.7 million Georgians covered by Medicaid and PeachCare. On its own, this process is a massive, complex undertaking. It places pressure on our state agencies and our health care system and could result in the loss of Medicaid or PeachCare coverage for an estimated 545,000 Georgians. The state also plans to roll out two additional health care programs during the Medicaid unwinding period.
In July 2023, the state will launch the Pathways to Coverage program, which partially expands Medicaid eligibility to adults who have lower incomes and comply with monthly work or other activity reporting requirements. Although Georgia’s enrollment estimates vary widely, the Governor stated that up to 345,000 people could qualify for the program.[1] In November 2023, the state also plans to transition to a state-based marketplace, which will affect the 825,000 Georgians who get their health insurance through the federally-facilitated marketplace. The state’s originally proposed Georgia Access Model program would have withdrawn the state from the federally-facilitated marketplace—which runs Healthcare.gov—without a state-based alternative. However, that program was suspended by the federal government in 2022 due to concerns over potential coverage losses. In February 2023, the state outlined a new plan for moving forward, and the state legislature passed SB 65 during Georgia’s 2023 Legislative Session. This legislation authorizes the Insurance Commissioner to establish a state-based marketplace.
activity reporting requirements. Although Georgia’s enrollment estimates vary widely, the Governor stated that up to 345,000 people could qualify for the program.[1] In November 2023, the state also plans to transition to a state-based marketplace, which will affect the 825,000 Georgians who get their health insurance through the federally-facilitated marketplace. The state’s originally proposed Georgia Access Model program would have withdrawn the state from the federally-facilitated marketplace—which runs Healthcare.gov—without a state-based alternative. However, that program was suspended by the federal government in 2022 due to concerns over potential coverage losses. In February 2023, the state outlined a new plan for moving forward, and the state legislature passed SB 65 during Georgia’s 2023 Legislative Session. This legislation authorizes the Insurance Commissioner to establish a state-based marketplace.
Without strategic investment and intentional planning, launching the Pathways to Coverage program and the state-based marketplace during Medicaid unwinding creates an unnecessary risk that could be harmful to those who depend on Georgia’s health care safety net, burdensome for state employees, and costly for the state.
Losses in coverage for Georgians with lower incomes
Some Georgians who lose Medicaid or PeachCare coverage during the unwinding may be eligible for premium tax credits that make marketplace plans more affordable. Launching the state-based marketplace in November—right in the middle of the 14-month Medicaid unwinding process—could make the transition to marketplace coverage confusing for both existing and newly eligible enrollees and would require intensive outreach to ensure enrollees are aware of the shift away from Healthcare.gov. Without having an opportunity to test new processes and work out potential kinks, the newly minted state-based marketplace would be taking on the re-enrollment of 825,000 existing enrollees during open enrollment from November 2023 – January 2024 while also transitioning those who lose Medicaid to marketplace plans during the special enrollment period from April 2023 through July 2024. All told, this creates the potential for decreases in coverage.
Increased administrative burden on state employees
Front-line staff at the Department of Human Services (DHS) handle the day-to-day work of determining individuals’ eligibility for Medicaid. The Medicaid unwinding places additional pressure on this historically underpaid and overburdened workforce. Once the Pathways to Coverage program launches, these same staff will also be processing the eligibility of newly eligible enrollees, including playing a role in handling the monthly reporting required of each enrollee. Although the full plan for the state-based marketplace has not yet been made public, the original proposal for the Georgia Access Model proposed leveraging both the existing Gateway system and potentially also DHS staff to assist with determining eligibility for premium tax credits for marketplace plans. Without additional intervention (e.g., pay raises), these added administrative burdens could harm morale and reverse the progress DHS says they have made on turnover rates.
Unnecessary or unclear state costs
Throughout the continuous coverage period, Georgia has received additional federal funding to keep Georgians enrolled in Medicaid. Although the Medicaid unwinding period does not end until June 2024, Georgia will go back to its standard federal match rate in January 2024. Because the Pathways to Coverage program does not qualify for the 90% enhanced federal match rate under the Affordable Care Act or the additional incentives offered under the American Rescue Plan, the state is passing up the opportunity to continue pulling down potentially billions in federal funds. The state will pay about five times more per newly eligible Pathways to Coverage enrollee compared to the state cost per newly eligible enrollee under full Medicaid expansion. Contrastingly, much of the state-based marketplace operating cost will be funded by user fees paid by health insurers who participate in the state-based marketplace. It is unclear, however, if additional state dollars are needed to fund start-up costs for the state-based marketplace, such as hiring staff support and building other in-house capacities.
Flawed Implementation of New Programs Would Compound Harm to Black and Latinx Georgians
Long-standing, racist policies and practices like regressive tax policies and occupational segregation have created inequitable access to economic opportunity for Georgians of color. Across the board, most non-elderly, non-disabled Medicaid enrollees work. However, low-income Black and Latinx Georgians are less likely than white adults to have access to employer-sponsored health care coverage and are overrepresented in Georgia’s Medicaid and PeachCare system.[2] Overall, about 1 in every 4 Black and Latinx Georgians are covered by Medicaid compared to about 1 in every 10 white Georgians. Among children who are 18 years old and younger (who make up a majority of the Medicaid and PeachCare population), about 1 in every 2 Black and Latinx children are covered by Medicaid compared to about 1 in every 4 white children.[3] This disproportionate enrollment means that these groups will also be disproportionately impacted by coverage losses during the Medicaid unwinding. This harm could potentially be compounded by the rollout of the Pathways to Coverage program and the flawed implementation of the state-based marketplace.
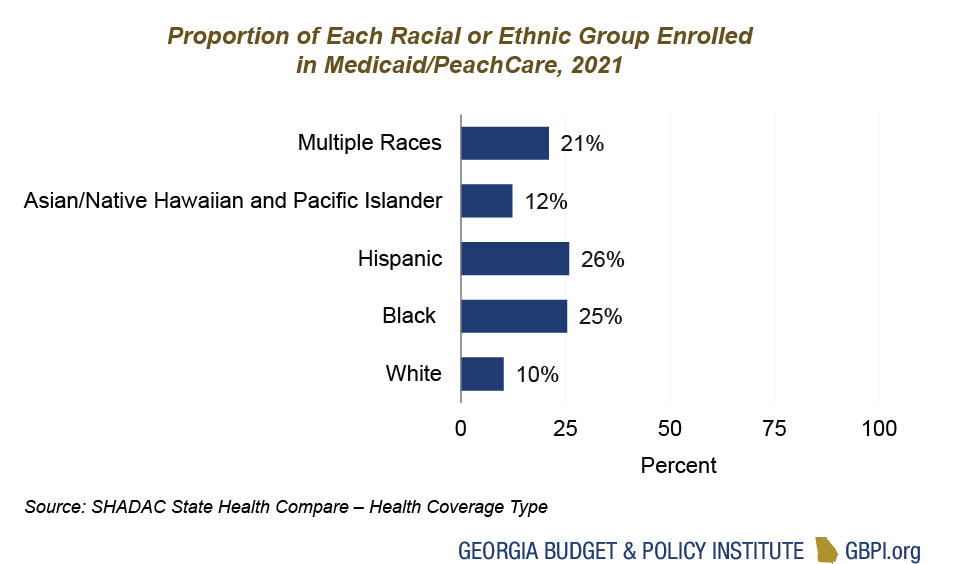
Source: SHADAC State Health Compare – Health Coverage Type
Some Georgians losing Medicaid eligibility during the unwinding—including mothers past their one-year of postpartum Medicaid and young adults aging out of Medicaid or PeachCare—may be eligible for Pathways to Coverage. Traditional Medicaid processes already make enrollment and eligibility harder for some groups. For example, one study found that Medicaid enrollees with limited English proficiency were five times more likely to lose their Medicaid benefits compared to those who spoke English. The Pathways to Coverage program’s monthly reporting requirements create additional red tape that could exacerbate inequity. For example, survey data show that Black and Latinx adults are less likely than white adults to own a computer or have access to the high-speed internet that may be needed to log into Georgia’s Gateway system and submit monthly documentation. This may mean that, although they are eligible, Black and Latinx Georgians may be less likely to remain enrolled in the program and thus become uninsured.
The transition to a state-based marketplace is not inherently harmful for Georgians of color who access health insurance through the marketplace. However, data show that intentional investment in outreach, education, and the navigator program are critical. For example, cuts to the federal navigator program funding during the Trump Administration led to significant decreases in coverage among people with lower incomes, Latinx adults, and people who spoke a language other than English at home. This will be particularly important for Georgians who lose Medicaid during the unwinding but qualify for marketplace plans. Without the right support, Georgians of color may be at risk for temporary, harmful gaps in coverage, which result in more trips to the emergency room and fewer filled prescriptions. One analysis found that Black adults moving from Medicaid to marketplace coverage had an average gap of 105 days compared to 73 days for white adults.
Delayed Marketplace Launch and Full Medicaid Expansion Could Help Expand Access to Health Care
Currently, there are 18 other states that run their own marketplaces, as well as other states considering making the shift. Those states cite potential benefits such as cost-savings, the ability to control insurance markets and reduce premiums, and generally more flexibility to meet state-specific needs. Moreover, integrated eligibility systems at the state-level can complement full Medicaid expansion by helping to reduce gaps in coverage when moving between Medicaid and marketplace programs. Despite the potential benefits, launching a state-based marketplace poses significant challenges, and Georgia would be the only state to run its own marketplace but not have closed the Medicaid coverage gap. During testimony for the 2023 legislative session, Georgians for a Healthy Future compared the state-based marketplace to a manual vintage Porsche and the federally-facilitated marketplace to a 2022 Honda Accord with GPS navigation. To ensure a successful marketplace launch that focuses on keeping Georgian’s covered, the state should delay implementation of the state-based marketplace and stick with the known and familiar federal marketplace until after the completion of the Medicaid unwinding.
The state should prioritize fully expanding Medicaid to help keep Georgians covered and minimize the human and fiscal costs of Medicaid unwinding. Rather than rolling out the costly and restrictive Pathways to Coverage program, federal financial incentives should be used to expand Medicaid eligibility to more people. Thanks to the bonus federal dollars offered under the American Rescue Plan, the state cost for full Medicaid expansion would be completely offset by federal funding for at least the first two years after expansion. Implementing Pathways to Coverage would cost more and cover fewer Georgians than fully closing the coverage gap. Moreover, young adults–including those 19, 20, and 21-year-olds who will be losing coverage during Medicaid unwinding and may struggle to comply with the reporting requirements of the Pathways to Coverage program–are the age group with the most to gain from full Medicaid expansion. It remains clear that all Georgians deserve access to affordable, high-quality health care, and closing the Medicaid coverage gap would put Georgia on the best path forward to achieving that vision.
End Notes
[1] Kemp, B. P. (2023, January 25). Governor Brian P. Kemp’s 2023 State of the State Address. State of Georgia website. https://gov.georgia.gov/press-releases/2023-01-25/governor-brian-p-kemps-2023-state-state-address
[2] SHADAC analysis of Health Coverage Type by Race/Ethnicity and Poverty Level, State Health Compare, SHADAC, University of Minnesota, statehealthcompare.shadac.org, Accessed April 25, 2023.
[3] SHADAC analysis of Health Coverage Type by Race/Ethnicity and Age, State Health Compare, SHADAC, University of Minnesota, statehealthcompare.shadac.org, Accessed May 1, 2023.